Breast Pathology (Inflammatory vs. Benign vs. Malignant)
393.38k views5102 WordsCopy TextShare
Dirty Medicine
SUPPORT/JOIN THE CHANNEL: https://www.youtube.com/channel/UCZaDAUF7UEcRXIFvGZu3O9Q/join
My goal ...
Video Transcript:
what's up everybody in this video i'm going to be teaching you everything that you need to know about breast pathology this is brought to you by dirty medicine if you want to support my mission to provide free quality medical education please consider clicking the join button which you can find as the first link in the description of any video on my channel as well as beneath any video on my channel if you click that join button you'll sign up to be a dirty medicine member where you pay 4.99 a month to support my channel financially
i thank you very much for your consideration now when it comes to breast pathology medical students freak out because there's a lot of different tumors a lot of different cancers a lot of different conditions they all sound alike they all involve the breast and for a lot of people keeping all these things straight memorizing buzz words recognizing histology and pictures it's just very difficult so i want to try to simplify this topic to put your mind at ease so that when you go into usmle and comlex you're feeling prepared to pick up some extra free
points now of course throughout this video i'm going to give you some really easy mnemonics to help conceptualize all of this and help with your recall so before i get started i just want to say that the purpose of this video is not to teach you pathophysiology the purpose of this video is to give you tools to answer questions and pick up points all right so let's get right into this before we get started i just want to give you a conceptualization of breast pathology and like how your brain should organize this when it comes
to breast pathology you want to separate it into one of three different categories we have inflammatory conditions we have benign conditions and we have malignant conditions we're going to go through each of these diseases one at a time but let me just give you the overview in the inflammatory conditions we're going to talk about mastitis mammary ductectasia and fat necrosis of the breast for benign conditions we're going to talk about fibrocystic changes intraductal papillomas fibroadenomas and the phylodes tumor and then for the malignant conditions we'll talk about ductal carcinoma in situ invasive ductal carcinoma lobular
carcinoma in situ and invasive globular carcinoma so each of these three categories represents a distinct grouping of pathology and we'll start with the inflammatory conditions and then just work our way down and then across to the right so that said let's just jump right in we're going to start by talking about mastitis so mastitis refers to inflammation of the breast parenchyma and you can see in this picture that you just get inflammation around the breast so i like to keep things stupid and simple anytime you see itis it's referring to inflammation swelling redness etc so
this itis is occurring in the mast or in the breast region and this is most commonly due to staph aureus and how this works is that a young mother will be breastfeeding and as she's doing that with repeated breastfeeding you get the formation of these little fissures on the breast and those little fissures are kind of like cracks in the skin and they give the staph aureus a route of entry into the breast and if that staph aureus enters into the breast it can cause localized infection hence the name acute mastitis now in addition to
breastfeeding and staph aureus entry into the fissures the other way that you can get formation of bacteria within the breast is due to insufficient milk drainage so when a a new mother is producing milk she either needs to breastfeed at a certain frequency or pump at a certain frequency which is literally like putting a suction cup on the breast and sort of sucking the milk out because the milk has to be relieved from the breast or else the milk will build up and back up and sort of clog that system when you've got a lot
of high nutrient milk clogging up the breast causing inflammation in the breast itself that's really just a nitis for bacteria so bacteria will feed off of those nutrients go to that area where the milk gets clogged up and backed up and you can also get mastitis that way so on u.s emily and comlex what you want to look for in the vignette is a mother that's breastfeeding that has a warm swollen tender breast and that could be either due to the entry through the fissures or it could be the same presentation with a mother that
they might say in the vignette like fell asleep for a prolonged period of time etc they're giving you clues that maybe mom forgot to pump maybe mom forgot to breastfeed so that's mastitis now when it comes to treating mastitis you use dicloxacillin analgesics and compresses now very high yield for step two level two and step three level three is they're gonna give you mastitis and they're gonna ask what mom should do and the answer is continue to breastfeed so even though it's gonna be very painful because the breast is swollen mom should continue to breastfeed
that's a very high yield point for step 2 level 2 and beyond so that's mastitis again itis meaning inflammation inflammation of the breast we talked about how it works how the bacteria enters and what the treatment is don't really need a pneumonic here because this is the only condition with itis so this is the one that's inflammation of the breast now let's talk about mammary duct ectasia so mammary duct dectasia refers to subareolar periductal inflammation with dilated mammary ducts the classic symptom that you see here is greenish brownish nipple discharge occasionally it can be bloody
but to make the question stem non-controversial usually the test writer will use this buzzword so it's going to be green brown nipple discharge if you see that you want to immediately think mammary duct dictation because that's the giveaway now this always can this also can present as a periareolar mass now when you see mammary duct dectasia they could describe what's known as an inverted nipple and you can google that if you want to see what that looks like this is thought to be due memory duct dectasia to endoluminal changes in the lactiferous system of the
breast that are associated with aging so as such you usually see mammary ductasia in like 40 to 50ish year olds possibly menopausal and again because these are due to changes that are associated with aging that endoluminal system changes and that leads to this peridoctyl inflammation and you get that classic dilation of the mammary ducts now again if you're sort of like what am i supposed to take out of this how will i pick this in a question green brown nipple discharge is the high yield buzzword that you want to know so with that said my
mnemonic to remember this is that you need you obviously need a way to know green brown nipple discharge so when i think of mammary duct ductasia i actually think of mammary duck ectasia and for me as a huge sports fan i'm sorry if you're not a sports fan this might be a little bit more challenging for you i think of the oregon ducks and their logo tells me a couple things one that greenish bronzish brownish orangish color i mean green is their main color but secondarily they've got that orange that green orange green brown if
you will that color is the color of the discharge so i always keep that in mind because mammary duck ectasia reminds me of the colors of the oregon duck the other thing is that the the bill of this duck up top i always think of that as being inverted which reminds me that if i see the word inverted nipple in the vignette i should also think of my memory duck ectasia so the oregon duck tells you a lot here gives you the colors of the discharge and if you think about its upper bill being inverted
it reminds you of an inverted nipple so again if you're not a sports fan you've never seen this logo before pick a different duck i don't know if other ducks have this color but this mnemonic worked really well for me now we'll talk about fat necrosis of the breast fat necrosis of the breast actually isn't that complicated but it's a test favorite because there are a lot of buzzwords that they can give you if they want you to pick fat necrosis of the breast so basically fat necrosis of the breast refers to non-viable adipose tissue
that gets replaced by scar tissue so basically something happens to the tissue in the breast which renders that adipose tissue non-viable or dead if you will and then our bodies just replace that with scar tissue which is sort of like a normal process in scar formation the only problem here is that it's happening in the breast and because it's happening in the breast and that's a very unique area of tissue you get these classic fat necrosis changes so what you'll see under the microscope is multinucleated giant cells with aberrant calcifications so those are buzz words
that you want to know for sure this is most commonly associated with one of two things this is where us emily or comlex is going to go they're going to give you a woman that experienced a mechanical trauma to the breast so some force was directed at the breast which basically killed that adipose tissue and then the body just replaced it with scar tissue and in replacing it now you see those giant cells those calcifications you can see what might mimic a malignancy because you can get the formation of a little mass there where that
scar tissue is being formed but it's just fat necrosis it's not breast cancer so it's either going to be mechanical trauma or the test will give you someone that recently underwent breast surgery and it was that local surgery basically rendering that adipose tissue non-viable that then caused fat necrosis to take place so you want to think trauma or recent surgery causing this fat necrosis which mimics malignancy but is not malignancy so big picture here is you need to know what's happening and what the buzzwords are because like i said there are a lot of buzzwords
that they can put in the vignette if they want you to pick fat necrosis so we need a mnemonic and when i think of fat necrosis of the breast obviously i'm thinking fat what has a lot of fat cheese and here you see a couple things you see a giant block of cheese that's full of calcium and that recently was cut with a knife what does this tell you well it's a giant block of cheese so it should remind you of multi-nucleated giant cells it's full of calcium so that should tell you about the calcifications
that you'll see in fat necrosis of the breast and it being recently cut by a knife reminds me of either recently being cut with breast surgery or recently experiencing mechanical trauma so fat necrosis of the breast what has a lot of fat cheese giant block of cheese that's full of calcium that was recently cut done all right so that's all the inflammatory conditions i flew through that this is sort of rapid review but again i'm giving you ways to conceptualize understand and use mnemonics to memorize what you need to know to pick out these these
answers on usmle and complex so now let's switch gears and talk about the benign breast pathology we're going to begin with fibrocystic change also known as fibrocystic disease of the breast now this is the most common benign breast pathology in this entire section so if you're taking step two level two or step three level three you wanna know that because that could show up as an epidemiology type question so when we talk about fibrocystic changes this refers as the name implies to benign fibrosis and cyst tissue formation look at the name guys it's fibrocystic fibro
means fibrosis cystic means cyst so fibrocysts fibrocystic changes occurring in the breast this is an umbrella term which refers to benign changes that occur in lots of different ways within the breast this usually occurs in premenopausal women so you're thinking people like 20 to 50 years old roughly and this is likely hormone-mediated so you want to know that pre-menopausal and hormone-mediated when it comes to taking or memorizing information about different types of tumors and cancers one of the ways that you can make a really educated guess is if you know the average age range because
some cancers only occur in post-menopausal and your elderly folks others occur in pre-menopausal and you're younger folks so if you knew that and literally nothing else you could make a very educated guess by eliminating possible answer choices so for fibrocystic change know that it's premenopausal and hormone mediated now what's really important to know about fibrocystic changes are these different subtypes because depending on what type of subtype of fibrocystic change which again recall that that's an umbrella term that refers to a lot of different histopathological changes that occur in the breast but depending on which subtype
we're talking about there's a varying degree of risk of the progression or the formation of cancer so there are three different subtypes and i'm trying to really keep this simple and the way that you should go about this is memorize that one is called apriocrine metaplasia one is called sclerosing adenosis and one is called atypical hyperplasia it's not important to know what those look like under a microscope i don't really think you need to know any other buzzwords of histopathology that are associated with them but you do need to know the names of these subtypes
and the degree of risk that they pose now i have a mnemonic here and i'll get into that in just one second but let me just read the normal first so apricorn metaplasia has no risk of cancer formation sclerosing adenosis has what they say some risk so they estimate that it's roughly um two times the risk and then for atypical hyperplasia there's very significant risk at least five times the risk so apocrine no risk sclerosing some risk atypical significant risk my mnemonic to remember this because this is very important very high yield is apok sclerosing
equals some and atypical is likely to a turn into cancer so for apocrine apo makes me think of your aok because there's no risk so instead of saying a okay i say you're apok so apocrine you're okay there's no risk sclerosing equals some so i just match those s's and then atypical can a turn into cancer so the a t in atypical is likely to a turn at in a turn into cancer because again with atypical hyperplasia of fibrocystic changes there's that roughly five times increased risk so if you see this on a test and
they say or describe apricorn metaplasia they say or describe sclerosing adenosis they say or describe atypical hyperplasia you need to know the risk associated with that so it's very important to understand so big picture here guys fibrocystic changes fibrocystic it's fibrosis and cis premenopausal women hormone mediated generally speaking it's benign unless you have either sclerosing so some risk or atypical can a turn into cancer if you're apocrine you're ape okay done let's move on now we're going to talk about intraductal papilloma an intraductal papilloma refers to papillary growth within the epithelial cells of a large
duct so as the name implies it's intraductal it's in the large duct now the way that this is going to present on us emily and comlex is going to be somebody with bloody nipple discharge it's likely going to be a pre-menopausal woman and then they're going to give you some histopathology and they're going to use the term fibrovascular projections the reason that this is a really tough question on usm elite and comlex is because intraductal papilloma is extremely similar in presentation and in histopathology to something known as papillary carcinoma both intraductal papilloma and papillary carcinoma
have bloody nipple discharge as the clinical symptom and fibrovascular projections as the histopathology so if you're given a question and the patient has bloody nipple discharge and fibrovascular projections lined by epithelial cells right now you don't know which of the two diagnoses you're dealing with so how do you get this right you have to look in the question and see or look at the image that they give you if they're going to be really tricky and c is there an underlying myoepithelium and if there is it's intraductal papilloma but if there isn't it's papillary carcinoma
so bottom line here is that both intraductal papilloma and papillary carcinoma will present with bloody nipple discharge and the histology will either be described as or show in the image fibrovascular projections lined by epithelial cells if there's a present myoepithelium it's intraductal papilloma and that is more of a benign picture and if there's no myoepithelium then it's papillary carcinoma now really briefly let's just talk about a myoepithelium because it's very important to understand and conceptualize so the myoepithelium as you see in this image is a physical barrier and that barrier is located above the basement
membrane and below the luminal epithelial cells and this serves a lot of functions in the prevention of cancer because this is literally a physical barrier between those epithelial cells that proliferate and turn into cancer and between the underlying stroma so if an intraductal papilloma were to theoretically break through the myoepithelium and then that myoepithelial layer is gone that's why when you look at the image and see no mild epi myoepithelial cells you're no longer dealing with intraductal papilloma you're probably dealing with something more invasive now the myoepithelial cells in addition to just being a physical
barrier also have tumor suppressor quality so they can induce apoptosis prevent angiogenesis and literally induce growth arrest in some of these cells that would otherwise go on to spread and become something more invasive than just intraductal papilloma so bottom line here is that the myoepithelial cells or the myoepithelium as a whole have a net effect of a physical and a chemical tumor suppressor so when we go back to this flow chart it should make a little bit of sense why you're trying to figure out in the image or by description is there a myoepithelium if
yes then this the papilloma is just intraductal it can't go anywhere because the myoepithelium is chilling underneath but if there's no myoepithelium then we're probably dealing with papillary carcinoma because unfortunately those proliferating cells have broken through so this is a very high yield discussion not only to get the answer correct when you're picking between these two breast pathologies but also just generally speaking to understand the role and the function of myoepithelial cells so going back to the slide that i started on this is intraductal papilloma now we need a mnemonic in order to to understand
and to memorize whether or not that myoepithelium is present and which disease that tells us we're dealing with so for intraductal i want you to think the myoepithelium is included so it's still there but for papillary that myoepithelium is popped so in papillary it's gone it's popped in intraductal it's included it's still there high yield just memorize this mnemonic this will take you very far now we need to talk about fibroadenomas so fibroadenomas are the most common breast tumor in women who are younger than 35 years of age fiber adenomas are marble-like non-painful rubbery mobile
benign tumors made up of stromal and glandular tissue really the big thing to memorize here and where i think the test writer will go on u.s emily and comlex is to know that fibroadenomas are estrogen sensitive so they actually have receptors on them that respond to hormones and therefore during pregnancy and during the menstrual cycle these fibroadenomas will get bigger and have the potential to exhibit some local symptoms like irritation uh pain etc generally speaking though they're not painful and then likewise since these are estrogen sensitive these tend to shrink and really not be any
issue whatsoever in postmenopausal women so if you're taking your test you've got a 15 to 35 year old woman and they describe a mass in the breast it doesn't hurt it has you know well-defined borders that sort of thing you want to think fibroadenoma so again only big thing to know here is that it's estrogen sensitive so my mnemonic is that fibro adenomas are estrogen sensitive if you know that mnemonic you're going to get most of your questions on fibroadenomas correct now the last major benign breast pathology we need to talk about are phylodes tumors
and to be honest fellowede's tumors can actually range from benign to malignant most of them are benign rarely some of them can be malignant these are fibril epithelial tumors again they range from benign to malignant really the big thing to know and where the test writer will go on usmle or comlex is to know that these have histopathological leaf-like projections into epithelial lines stroma in dilated lumen you can see the image at the bottom of this slide it's pretty characteristic when you're looking at breast tissue that you see those leafy looking projections these usually occur
in 40 to 50 year old women perhaps knowing that age range can help you eliminate some answer choices but for your fellowes tumors you just want to remember those leaf-like projections my mnemonic here is actually super simple and helpful when you think leaf-like projections i want you to think leafy-like leafy-like for phyllodes leafy-like projections you just need to know that buzzword because this is what's going to show up either that image is going to show up or that buzzword is showing up if they don't give you any of those things there's absolutely no way that
you're going to get felodi's tumor correct on your usmle or complex so with the completion of the floaties tumor we've now gone through both inflammatory conditions and mostly benign conditions we're now going to conclude this video by talking about the malignant breast pathologies truth be told the malignant breast pathologies are not that difficult to memorize and you'll see in just a second but there's not a lot of buzzwords there's not a lot of really highled things that are associated with the malignant conditions so for that reason these are a little bit easier to learn although
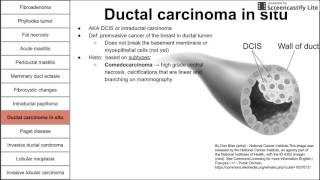
they're still difficult to memorize because they do sound quite similar so let's get started with ductal carcinoma in situ so in situ just generally speaking for those of you who like to understand language to understand what you're dealing with on tests in situ means it's like in the original place it hasn't left so if it's ductal carcinoma in situ yes it's ductal carcinoma yes it's technically malignant breast cancer but it hasn't yet invaded the basement membrane so generally speaking when you see in situ you know that whatever carcinoma it's talking about if it's that in
situ it's that not yet through the basement membrane so ductal carcinoma in situ is proliferation of the cells within ducts hex hence the name ductal carcinoma but since it's in situ has not yet invaded the basement membrane and that's actually important to understand because if they give you an image and you're able to see the basement membrane in that image and see that there's no cells breaking through there and no growth that looks dysplastic or what have you beyond that then you're in good shape the the one thing that does pop up with ductal carcinoma
in situ is the presence of calcifications in a lot of different arrangements so i think you need to know the ductal carcinoma in situ has calcifications so ductal carcinoma in situ for me is dcs dcs has dem calcifications dcs ductal carcinoma cyto dcs dem calcifications i don't know how to emphasize the s at the end of a word that's so awkward hearing me do that out loud um but that's it for ductal carcinoma in situ so then we have invasive ductal carcinoma and whenever you have invasive blank you can think of the blank as being
the in situ version but now we've broken through the basement membrane so invasive ductal carcinoma is basically you can think of it as dcis once we get through that basement membrane and now the prognosis is obviously worse so this has duct-like structures in a desmoplastic stroma if you see that description they're talking about invasive ductal carcinoma now there are a few subtypes of invasive ductal carcinoma that you need to be familiar with or at least be able to recognize the first big one which is going to be the second image on the bottom of the
slide is medullary breast carcinoma and medullary breast carcinoma can be described as a sensational sheet-like growth with lymphocytic infiltrate so you look at that second image you see all those lymphocytes you see the relative sheet-like growth that's going on that's medullary breast carcinoma being somewhat of a subtype of invasive ductal carcinoma the third image i want to show you and the highest yield subtype for exam purposes is inflammatory breast carcinoma the reason that this is the highest yield subtype is because the image is the most unique and the description is the most unique so this
is going to be described as dermal lymphatic invasion by tumor cells and the way that it could present in the vignette and where i think the test writer will go is they're going to describe somebody with a unilateral painful swollen breast and you're going to have to pick between invasive ductal carcinoma or more specifically inflammatory breast carcinoma you're going to have to pick between that and mastitis because this is gonna look a lot like acute mastitis and the the way that you're gonna pick this is either by the image which you see on the far
right and i'm i'm gonna butcher this but that's known as pio de orange i think that's french please excuse my butchering of the word um so it's it's described to look like the skin of an orange peel down orange am i saying that right someone let me know in the comment section um if the breast looks like the skin of an orange you're dealing with inflammatory breast carcinoma and you're also going to look for the description obviously so if they talk about lymphatic invasion specifically dermal lymphatic invasion then you're dealing with inflammatory breast carcinoma and
not necessarily dealing with acute mastitis recall you know we went through this conversation earlier in this video if they want you to pick acute mastitis they're going to give you someone that's breastfeeding or someone that didn't uh get the milk out of their breast by pumping or by breastfeeding so the risk factors are a little bit different as well so that's inflammatory breast carcinoma that third image is extremely high yield know what it is what it's called in french hopefully you can say it correctly because i certainly can't and know the description so that's invasive
ductal carcinoma now just like dcis and then invasive ductal carcinoma we also have lcis lobular carcinoma in situ so what is this well it's lobular so it's proliferation of lobular cells and it's in situ so it's not yet invaded the basement membrane funny how language works huh guys now the big thing here is that this lacks e-cadherin all right so that's very high yield because e-cadherin has an adheren excuse me as an adhesion protein is very important for preventing certain type of cellular derangement so lobular carcinoma in situ lcis really what you need to know
is that it lacks e cad here and that's like singularly the only high yield fact that i need you to know so because of that you want to think that lobular carcinoma lacks cadherin lc lc lobular carcinoma lacks catherine now if lcis were to theoretically break through that basement membrane now you're dealing with invasive globular carcinoma all right so i'm just trying to simplify this this is basically lcis through the basement membrane and just like the in situ version this lacks e-cadherin and the way that this will be described to you and this is the
yield point for invasive lobular carcinoma is that it is non-cohesive cells organized in a single file pattern and i'm sure that if you look at this image you can appreciate that this looks very distinct from the other images of the breast cancers that you've seen so that single file pattern of cellular organization is very unique to invasive lobular carcinoma so we need a mnemonic to remember this so when you think of invasive lobular carcinoma i want you to think of ilc ilc for individual line carcinoma which reminds me of single file pattern individual line carcinoma
for single file pattern it's very important to understand because that image is pretty high yield great news everybody we're done we've gone through the inflammatory conditions the benign conditions and the malignant conditions again the emphasis of this video is not to teach you pathophysiology the emphasis of this video is to teach you how to use clever mnemonics tips and tricks to conceptualize to simplify and to get extra points on usmle and comlex so i hope that this was useful to you if it was please like and subscribe share it with your buddies good luck keep
it up
Related Videos
30:19
Lung Cancer/Tumors
Dirty Medicine
167,280 views
14:34
Testicular Cancer/Tumors
Dirty Medicine
117,036 views
14:36
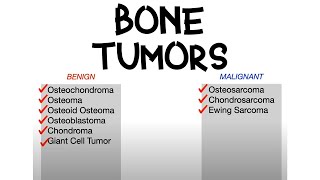
Bone Tumors (Benign vs. Malignant)
Dirty Medicine
305,767 views

27:01
Thyroid Disease (Hyperthyroidism vs. Hypot...
Dirty Medicine
150,497 views

1:28:55
#PATHBOARDS High Yield Breast Pathology fo...
pathCast
13,818 views

21:19
Estrogen Receptors & HER2/neu Receptors i...
Oster Oncology
66,020 views

2:17:12
The Speaking Coach: The One Word All Liars...
The Diary Of A CEO
2,298,210 views
22:44
Lower Extremity Nerve Injuries
Dirty Medicine
352,750 views
34:34
Anemia (Types, Findings, Lab Values)
Dirty Medicine
352,709 views
27:38
Lymphoma
Dirty Medicine
10,864 views
3:38
Understanding Breast Cysts - with Dr Tasha
Dr Tasha
62,683 views
11:21
Diseases of Breast: Part 1. Normal anatomy...
ilovepathology
163,228 views
26:57
DCIS - A Pathologist's Perspective | 2023 ...
Dana-Farber Cancer Institute
46,227 views
15:17
Understanding the Immune System in One Video
Zero To Finals
1,561,841 views

1:01:16
Oncology Series | Breast Cancer - Molecula...
Unacademy Live - NEET PG
160,789 views

28:46
HIV Medications/Drugs
Dirty Medicine
288,908 views
19:05
Brain Tumors
Dirty Medicine
386,990 views
27:59
Endometrial Cancer | Risk Factors, Pathoge...
JJ Medicine
229,798 views

15:52
Hydrocele vs. Varicocele vs. Torsion vs. E...
Dirty Medicine
755,847 views
21:30
Female breast pathology
MedLecturesMadeEasy
100,722 views