Temporary Pacemakers - Modes and Basic Settings
172.13k views5992 WordsCopy TextShare
ICU Advantage
We continue the series on Temporary Pacemakers and take a look at the different modes they operate i...
Video Transcript:
all right you guys welcome back to another video lesson my name is eddie watson and this is icu advantage where i'm giving you the confidence to succeed in the icu by breaking down these complex critical care subjects and making them easy to understand for you and if you'd be interested in getting these critical care lessons on a weekly basis then i invite you to subscribe to the channel down below when you do though make sure you hit that bell icon and select all notifications that way you're never going to miss out when i release a
new lesson now in this lesson here today we're going to be talking about the different modes that we have for our temporary pacers as well as covering some of the basic settings and sort of basic operational information in order to be able to effectively manage a patient with a temporary pacemaker at a minimum you need to understand the differences between these modes as well as the basics for the operation of this pulse generation so make sure and keep watching because i've got a lot of great information for you guys all right so here we are
continuing our discussion talking about temporary pacemakers so in this discussion the first thing that i actually want to talk to you guys about are the different modes that we have for our pacing now the way that a pacemaker operates is based off of three primary things where it's pacing where it is that it's sensing the intrinsic rhythm from and then what to do if a sensed beat is detected now there's a nomenclature that we use in order to be able to tell us all three of these things and then how this pacemaker is actually operating
there's basically a three-letter code that is going to tell you what type of operation that pacemaker is currently operating in in order to help you remember what each one of those letters stand for it helps if you can remember the acronym psr and this is going to stand for paste sensed and response all right so let's actually talk about these so they make a little bit more sense now paste i think is pretty self-explanatory this is going to be where is this pacemaker pacing and so then for this first letter we have three options to
choose from a v and d now a stands for the atrium v stands for the ventricle and d stands for dual or both chambers and so what this is telling you is if the first letter in the three-letter mode setting for our pacemaker is an a this means that we're sending pacing to the atrium if it's a v it means that we're sending pacing to the ventricle and if it's d then it means that we're sending pulses to both the atrium and the ventricle all right so that's our paste now the second letter is going
to be our sensed and here we're actually going to have four letters a v d and o now here again a is atrium and v is ventricle and then d stands for dual and o means none and so what we're talking about when we're talking about sensing is the pacemaker's ability to pick up on the intrinsic heart rhythm and so in the cases here are we sensing that rhythm from the atrium the ventricle are we looking at both of the chambers here or are we not doing any kind of sensing and the sensing plays an
important role in the third letter of our mode setting that's going to be our response which is this is our response to a sensed event now for a response we also have four different letters that we can use here we have t i d and o now t stands for triggered now in order for me to explain about triggered actually helps if i mention what the i stands for and the i is inhibit this is also something that we refer to as demand mode and the reason for this is the reason we call it inhibit
is because when it senses an intrinsic heartbeat that it's going to inhibit the pacer from firing so if it senses that the patient has a heart rhythm it's not gonna fire the pacer and it's only gonna fire the pacer whenever it's needed or demanded now going back to triggered triggered means that we're gonna trigger an action whenever a intrinsic heartbeat is recognized without any inhibition now this might not make a whole lot of sense i'll kind of try to loop back to this and sort of fill in the gaps but the important thing to know
here is that having a pacer in the mode of a t response actually has no clinical application when it's only triggered alone to try to explain that a little bit better let's actually move on and talk about the d which stands for dual and this means when it senses an event that it can both inhibit and trigger an action and just a really quick example to to make this make sense for you guys if it senses a beat in the ventricle it's going to inhibit the pacer from firing because the heart is already contracting whereas
if we maybe sense a beat in the atria that this could trigger the pacemaker to send a pulse to the ventricle so depending on what mode we're in and where we're sensing this intrinsic heart rate that this is going to determine what we're going to do with it so going back to that t triggered well it makes sense sometimes to have a triggered response to trigger without any sort of inhibition really doesn't have any clinical application and then finally we have o which again stands for none and this means we're basically not going to have
any kind of response to any sort of sensed event and so in fact we're only going to see an o for the third letter when we also have it for the second letter basically meaning we're not doing anything with sensed beats we just essentially have the pacemaker firing and so this is why this is also referred to as asynchronous now on that topic i actually do want to talk about the difference between asynchronous versus synchronous pacing and so we can either have the pacemaker operate in synchrony with the patient's intrinsic rhythm or the pacemaker can
operate independently operating independently means we're not sensing the underlying heartbeats and this is what we refer to as the asynchronous and if we are working in synchrony with that intrinsic rhythm this is where we were talking about having the demand mode we're either going to send pulse generation to the heart and not care about what the heart is doing underlying or we're going to sort of listen to or sense those intrinsic heartbeats and then based on what sense determine whether or not we need to give a pulse generation now again it's important that you understand
that because operating an asynchronous mode means that we're going to continue to fire without any regard to what the heart is doing on its own now we know that the heart's only going to contract when the ventricle is not in its refractory period but if it's outside of that refractory period and we're just sending pulse generations whenever we want we really run the risk of triggering a beat during the repolarization that are on t event when we're operating in this mode and this could trigger ventricular fibrillation which obviously is not going to be good for
our patients so in almost all cases with the exception of some pretty within the icu some pretty infrequent situations to encounter we're almost never going to use asynchronous mode and this is only something that we want to be using on patients who are fully dependent on their pacer so as i go through i will talk about some of these specific asynchronous modes but again just realize that the chance that you're going to be using one of these is probably pretty slim all right so with that stuff out of the way here the next important thing
for us to talk about is going to be the difference between our single chamber and our dual chamber pacemakers and so just as we had in the intro here is a picture of a couple examples these happen to be the medtronic the newest version of the medtronic temporary pacers we have on the left is actually our dual chamber pacemaker and then on the right is the simpler single chamber and so let's actually start off talking about the the more simple one the single chamber now this one as the name suggests can only sense and pace
a single chamber of the heart either the atrium or the ventricle now like i said this is simpler to operate as there's really less modes available to us and less settings to have to change as you can see looking here at this example we just have the three knobs or the dials to be able to change then just a couple buttons so not a whole lot of settings to deal with here now like i said there's only a couple modes that we have available on here and really these modes are going to be dependent on
where it is that your pacer leads are going to if you have leads going to the atrium you're going to only have two different modes that are related to the atrium to choose from and then if your leads are then going to the ventricle then you only have two different ventricular modes to choose from so we'll actually start off talking about our ventricular modes and there's two different modes we have vo and vvi so let's actually work through these first to a little bit slower if you remember that acronym prs paste sensed response so in
this first one for voo the first letter is a v which means we're going to be pacing to the ventricle the next two letters though both for sensed and response are o and if you remember that means none so this means we're not going to be doing any sensing and there's not going to be any response to something that we're not even sensing and so this means that this is actually our asynchronous mode and again isn't going to be one that you're probably going to use a whole lot now for this other mode vvi so
again we know we're pacing in the ventricle now for the next letter the sense that this is a v so this means we're going to be sensing from a ventricle and if you think about it it kind of makes sense we only have one pacer wire so we're gonna have to be sensing in the same place that we're pacing now for the third letter this is the response to a sensed event and here this is gonna be an i and this means inhibit and so this tells us that when we sense a ventricular beat we're
going to inhibit the pacemaker from firing a beat makes sense if the heart's already contracting we don't need to send a paste beat to it we only need to do that when it's not and so again this is going to be a demand mode and actually vvi is one of the two most common modes of pacing that you're potentially going to see now both of these two modes when they're operational is something that we refer to as being v-paced and so let's actually take a look at a rhythm of what a patient who's being v-paste
is going to look like so as you can see here we have our pacing spike which is going to be from our pacemaker firing and you can see each of those right along here now following the pacer spike we have our ventricular beat which you can really kind of tell that because it's a little bit wider almost like you'd see a pvc again because we're not using the fast paths of those bundle branches and purkinje fibers to to send that signal around now in this example here every single beat of the patient's heartbeat is coming
from a pacer generated pulse which basically tells us that either the patient's heart rate is lower than what we have this pacemaker set at or they just don't have any intrinsic heart rhythm to begin with but like i said in vvi we're actually working in demand mode and so this means we're not always going to be giving a a pulse generation it's going to be based on what the patient's underlying rhythm is so here's an example of that and so in this example here you can see our first couple beats are actually normal beats we
don't see any pacer spikes but then after that second one a long enough period of time goes by that the pacemaker needs to then kick in in order to maintain the rate that it's set at so we have a few beats that go along that are paced and then the patient's intrinsic heart rate picks back up and we go back into the the normal rhythm that you see so here we're sensing for those intrinsic beats so when the pacemaker sees them it's going to inhibit that pulse generation until it gets to the point where that
it no longer senses it and then it's going to kick in and send those pulses or that stimulation to the heart muscle but then after each beat it's going to continue sensing and if it senses it again then it's going to go ahead and inhibit once again like we see at the end now vvi again remember that this is a single chamber mode so so just to recap that we're going to be sensing and pacing in the ventricle now important to know with this is that it will not necessarily be in synchrony with the atrium
contracting if the patient is in a sinus rhythm and so since we're only pacing the ventricles we're often going to see a decreased cardiac output because we're going to be losing that atrial kick and so this may require running the rate a little bit higher than we normally would think to so those are our two ventricular modes now let's talk about our two atrial modes and these are very similar ao and aai and again these are what we're going to be referring to as being a paste and so again let's bring up an example of
what just straight a-pacing looks like and so here again we can see our pacer spikes right along here but this time you can see that the the spike is actually preceding a p wave and then following that p wave we actually have normal looking qrs complexes so now hopefully the naming convention is starting to make a little bit more sense here so again we have aoo that means we're not sensing or responding to any kind of sense event which means that again this would be our asynchronous mode and then aai means that we're now sensing
in the atrium along with pacing and the atrium again duh makes sense we only have that one lead and then our response to that sensed event is to inhibit which means this is our demand mode and so let's actually take a quick look at that one here so again at the beginning we can see our normal patient rhythm that's going there after the second beat we have a long enough delay that this is going to trigger the pacemaker to fire but now we have an atrial paste beat and so we're going to see that normal
morphology p wave and then followed by a normal qrs complex so we have a couple of those beats but then we see that the patient's intrinsic rhythm picked back up in time so our pacemaker sensed that and didn't send an atrial pacer spike but then again it had to do it again here at the end and so then just for clarity's sake we know that this is going to be sensing and pacing in the atrium we're gonna have that normal p wave and qrs complex morphology but an important distinction here is that we and hopefully
that makes sense to you guys why that is because here we're only sending impulses to the atrium we're not sending anything to the ventricle this is just a single chamber pacemaker so if there is no intrinsic heartbeat and we send that pulse to the atrium it will cause contraction in the atrium but if there's no conduction through the av node we're not going to pass that signal onto the ventricle and we're not going to get any sort of heartbeat so really important to know we can't use that here so those are our single chamber pacemakers
as you can see we just have really kind of two options vvi or aai because again we're probably not going to be using one of the asynchronous modes pretty simple are we pacing in the ventricle or pacing in the atria and so now let's actually move on and talk about our dual chamber pacemakers now here again you can see another example of this here and you hopefully can see how much more complex this potentially is going to be than just the single chamber pacemaker we've got a few more dials and knobs and there's actually a
whole other screen which is going to displace additional settings for us on here and the reason for this is because that this particular pacemaker is going to offer the greatest flexibility in our pacing options for our patients and part of the reason for this is we can with a dual chamber pacemaker operate in single chamber modes just as like we just talked about but using this particular pacemaker if we have atrial and ventricular wires present then this is going to open up even more modes for us to work with and so having both of those
pacing leads is going to open up three additional modes for us we have d o o d d i and d d d and all of these modes would give us something that we refer to as av paste and so again let's take another quick look at what that would look like here and just as the name suggests and the first letter that we see in the mode nomenclature is a d which we know means dual or both chambers so all three of these modes start with that d which means we're going to be pacing
both the atria and the ventricle and so here we can actually see pacer spikes and you have a set of pacer spikes for each heartbeat now in this example here the first pacer spike is our atrial pacer spike which is then preceding the p wave causing the atrium to contract and then the second pacer spike is our ventricular pulse which is then preceding a wider qrs complex and is triggering that ventricular contraction and so again hopefully looking at the names of these modes that this is starting to kind of sink in for you guys so
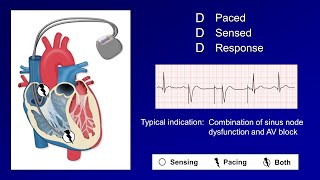
again doo means we're doing dual chamber pacing but we're not doing any sensing or any obvious response to a sensed event so this is going to be our asynchronous mode and i'll actually come back and explain what ddi is because it's going to help to understand ddd to better understand ddi which is a little bit different than what we've just been dealing with because in the single chamber pacemaker the most common mode that we used was the inhibit mode either vvi which is the most common or aai but here in our dual chamber pacing ddd
is going to be the other one of those two most common modes that we use so here again we know that this mode senses and paces in both chambers now the important distinction here is that final letter so we know we're doing dual chamber pacing dual chamber sensing and dual mode of a response to that sensed event which if you remember means we're either going to inhibit or trigger and so what it does when it senses a beat is really going to depend on which chamber it is that it senses so if neither the atrium
or the ventricle is sensed it's going to deliver a stimulus to the atrium followed by a delay and then to the ventricle now if the atrium is sensed that this is going to inhibit our atrial stimulus from being sent and so the pacemaker is going to continue to be sensing now in the ventricle but if after a specified period of time there is no ventricular beat then the sensed atrial beat is actually going to trigger a stimulus to the ventricle so hopefully this makes sense if we sense that the atria has contracted we're not going
to send a another pacer spike to the atrium but we're going to wait and give it time and see if that signal actually propagates to the ventricle if enough time has passed and it hasn't then we need to stimulate that ventricle to contract and then finally if the ventricle is sensed regardless if there was an atrial sensing or not then both the atrial and ventricular leads are going to be inhibited from sending a stimulus and this is really the meat and potatoes of that last d that responds to a sensed event because that same sensing
can either inhibit the atrial pacing or it can be used to trigger the ventricular pacing and so it's really doing both modes so again if it senses in the ventricle it's just going to be inhibiting here there's no triggering happening and so with that explanation out of the way for ddd it helps to make the understanding of ddi a little bit easier because this one's similar to ddd except the only atrial beats that are gonna trigger ventricular stimulation are gonna be ones that we provide so the paste atrial beats and the whole purpose of this
is it's going to prevent high ventricular rates in patients with proximal afib so in the case of afib where that atrium is just contracting at a very high rate if every single one of those was passed along the ventricle we would have a very high ventricular rate so we wouldn't want that happening so we're actually going to inhibit that from from taking place and then the only time that we're going to have a atrial beat that we sense it's then going to trigger a ventricular beat is if it's one that we provided the stimulus for
so we can actually control that proper rate so now interestingly the the pacing example that i showed you here this was just a 100 percent av paste i did want to actually show you another example that's going to show us several different types of paste beats that we can see for a patient and a pacer mode of ddd all right so number one this is going to be just our normal intrinsic patient heartbeat pretty self-explanatory now number two here this is gonna be one where enough time elapsed and we did not sense an atrial beat
so we sent an atrial pacer spike but then again we waited and enough time went along that we didn't see a ventricular beat so then we also triggered into a ventricular beat now in example number three here this example again enough time went along that we didn't see an atrial contraction so we had to send a pulse to stimulate atrial contraction but this time that atrial contraction and that depolarization made it through the av node and onto the ventricle in enough time so then we see that we have a normal qrs complex and no second
pacer spike and then finally in our fourth example here in this example the patient ended up having their own intrinsic atrial contraction but as enough time went on we didn't see that ventricular response so the pacemaker then used that sensing of the atrial contraction to trigger the pulse generation causing contraction in the ventricle so kind of crazy that we can see four different types of of beats and patients who are in a dual chamber pacemaker set in ddd all right so that's the big difference between the single chamber and our dual chamber pacemakers and the
different modes that we have available to us in there and so now lastly let's actually talk about some of the basic settings that we have now this isn't going to cover all of the settings that we see on the pacemaker i'm actually going to have a separate lesson that's going to go more in detail into some of the more advanced if you will settings that we can change on the pacemaker but these are going to be the most basic ones that you really have to understand if you want to be competent and caring for patients
with these pacemakers and the first thing is that we're going to talk about is going to be our rate and this one's really the the simplest of these settings that we have essentially it is the rate at which you want to pace your patient's heart rate and so if our patient's intrinsic heart rate drops below this set right here then the pacemaker is going to stimulate a contraction now interesting though is that the the pacemaker actually works off of timing so instead of measuring the beats per minute like we normally do when we look at
things it actually measures how much time has taken place since the last event and this time is actually measured in milliseconds and a simple example is as if we have a patient who has a heart rate of 60 beats per minute this means that they have one beat every thousand milliseconds or more simply they have one beat every second and so if we then had our pacemaker set with a rate of 60 then if a thousand milliseconds or one second has gone by and it hasn't had another sensed event then this is gonna trigger the
pacemaker to fire a pacing spike so pretty straightforward other than the fact that it's just looking at the time that takes place between each beat so the next important setting that we're gonna have on our pacemaker is gonna be our mode now in our single chamber pacemaker you're not gonna have a direct way of changing the mode obviously if your pacer lead is in the atrium you're gonna have an atrial paste and sensed beat and if your lead is in the ventricle then you're gonna have a ventricular sensed and paste beat but you do have
ability to change the synchrony so again think your ao versus aai or voo versus vvi and basically the way that you activate this asynchrony is to turn the sensitivity all the way up until you reach that asynchronous mode now on the dual chamber pacer you've got a long list of modes that you can choose from and again they can operate in single chamber modes as well as the dual chamber mode so you've got aoo aai voo vvi ddo ddi and ddd now on the dual chamber pacers you can either just set this directly or there
are some things you can do to actually trigger it to go into one of these modes so again if you're in vvi let's say so your ventricular sensing and ventricular pacing uh but you turn the sensitivity all the way up just like you did on the single chamber pacemaker that's gonna put you into asynchronous mode which is by doing that flipping you into vo now so there are some ways to do that with some of the settings on the dual chamber pacers which i'll probably talk about in that other lesson where we go a little
bit more in depth into some of the more advanced settings but i do want to move on next from here and actually talk about the next setting which is going to be our output all right now the output this is going to be a measure of the stimulus pulse generated in milliamps now the point of our output is to stimulate capture and capture is going to be defined as the stimulus leading to a contraction of the heart now if our milliamps are not high enough to stimulate this contraction then no capture is going to be
present now to understand this concept there's something that we have that we call the stimulation threshold and this is essentially the minimum output in milliamps that's needed to consistently lead to capture and it's important to know that this isn't always just a fixed value so age of the leads drug therapy that the patient's on their acid-base status that this can all impact this stimulation threshold and so because of some of these fluctuations if possible we want to try and maintain what we call a 2-1 safety margin above our threshold so this way we know that
if some of these values change and this threshold becomes higher that hopefully we've have our output set high enough that even with those changes we'll still continue to get capture and so fortunately there are some pretty simple steps in order to figure out what this stimulation threshold is so the first is we want to set the rate at least 10 above what our patient's intrinsic rate is then we want to decrease the output so this is our milliamps until we have the loss of capture now when you do this you're going to be seeing the
pacing and the sensing lights flashing intermittently now from here we want to increase the output slowly until we have consistent capture and so this here is going to be our stimulation threshold and so finally once we know this threshold we want to set our output two to three times this threshold all right and then finally the last setting that i'm going to talk about is going to be our sensitivity and so when we talk about sensing like we said this is the pacemaker detecting the patient's intrinsic heart rhythm sensitivity then is the measure in millivolts
of the required amount of electrical energy needed to detect that heartbeat now this particular setting often confuses people the higher the sensitivity the less likely that the pacemaker is to see the patient's intrinsic rhythm and so to help you kind of understand this a little bit better let me put up a strip with a just basic sinus rhythm on here and so we can really think about our sensitivity kind of like a fence now in the case where our sensitivity is too high the fence is too high and as you can see you can't actually
see any of the intrinsic heart rate but if we're lowering that sensitivity and we lower it just enough then we can get it to the point where we can just see the patient's intrinsic heart rhythm continuing along if you lower it too much then it's going to start to see every single thing in there and consider all of that the patient's intrinsic heart rhythm so again like i said the higher the sensitivity the less likely the chance that we are going to have our pacemaker seeing the patient's rhythm now once again similar to our output
for our sensitivity we actually have something that we call our sensing threshold and this is going to be the least sensitive millivolt setting in which the temporary pacemaker can detect a heartbeat now again the age of the leads the drug therapy patient's acid base status that this can all affect this threshold and again if possible we want to try and maintain that two to one safety margin below this threshold so once again we do have some steps in order to help us determine what this sensing threshold is now important to know though that you only
want to perform this if your patient has a sufficient intrinsic heart rhythm underlying so first we want to set our rate 10 below the patient's intrinsic rate next we want to turn the output all the way down to 0.1 milliamps then we want to start decreasing the sensitivity until the sense indicator light stops flashing now when the sensing indicator light stops flashing we're going to have the pace indicator light which is going to be flashing but at this point we're not going to have capture likely because we have the output set to just 0.1 milliamps
now here we want to increase our sensitivity until the sense indicator starts flashing this is going to be our sensing threshold then in order to maintain that safety margin we want to set our sensitivity to half or less of what this threshold is and then finally most importantly restore the rate and the output to the previous values and that is our sensitivity those are the basic settings that you really have to understand when you're operating a pacemaker for your patient and then overall that's this lesson covering the different modes and settings at the the basic
level that you really need to understand in order to be competent and being able to take care of a patient that you find yourself with that has a temporary pacemaker so i really hope that you guys enjoyed this lesson if you did please leave this lesson a like go down in the comments leave me a comment let me know what you thought and make sure and share this lesson with other people that you think might also enjoy it as well as if you haven't already make sure and subscribe to the channel down below there as
well a special shout out to our youtube members and patreon members out there the support that you guys offer for this channel really goes a long way in allowing me to continue to do bigger and better things for this channel moving forward into the future uh so a big thank you to you guys now for the rest of you guys if you'd be interested in showing additional support for this channel you can either join the youtube channel membership down below or head on over to the patreon page and check out some of the extra perks
that you get for doing just that as well as you can always support this channel by following the links that i have down in the description or checking out some of the really awesome t-shirt designs that i have linked to just below this lesson here make sure and stay tuned for the next lesson in this series but in the meantime make sure and check out a couple really awesome lessons i'm gonna link to right here as always thank you guys so much for watching have a great day
Related Videos

14:01
Additional Settings for Temporary Pacemakers
ICU Advantage
26,045 views

11:12
An Introduction to Temporary Pacemakers
ICU Advantage
151,435 views

24:49
Targeted Temperature Management (TTM) - Th...
ICU Advantage
67,712 views
19:06
Pacemaker Modes and Settings
Strong Medicine
242,992 views

19:19
Troubleshooting Pacemaker Problems EXPLAINED!
ICU Advantage
57,470 views

18:23
The BASICS of the Pulmonary Artery Catheter
ICU Advantage
197,232 views

1:45:06
The Complete ECG Rhythm Interpretation Ser...
ICU Advantage
16,574 views

24:41
Basic Vent Modes MADE EASY - Ventilator Se...
ICU Advantage
1,701,712 views

19:33
The SHOCKING Truth | Defibrillate, Cardiov...
ICU Advantage
334,721 views

16:34
Pacemakers
Ninja Nerd Nursing
18,081 views
8:46
Temporary Pacing Threshold Checks
The Alfred Intensive Care Academic Centre
2,354 views
20:40
VV vs VA ECMO Explained!
ICU Advantage
181,862 views

7:41
Medtronic Transvenous Pacemaker
Janis Provinse
49,640 views

39:22
Cardiac Arrest Rhythms - A Quick ACLS Review!
Pass with PASS
16,854 views

9:25
Sensing and Threshold Test — 53401 Tempora...
Medtronic Cardiac and Vascular
207,486 views
33:02
The SIMPLE Steps of 12-Lead EKG Interpreta...
ICU Advantage
76,051 views

9:30
Temporary Epicardial Pacemakers and Sensit...
The Alfred Intensive Care Academic Centre
20,213 views

1:22:41
The Comprehensive ACLS Review Series!
ICU Advantage
38,038 views

7:04
Placing a Transvenous Pacemaker
EM:RAP Medical Education
206,721 views

19:21
Metabolic Panels and Electrolytes - BMP vs...
ICU Advantage
143,889 views