Most Common ECG Patterns You Should Know
1.54M views1608 WordsCopy TextShare
Rhesus Medicine
We look at the most common ECG rhythms and patterns seen in Medicine, including main identifying fea...
Video Transcript:
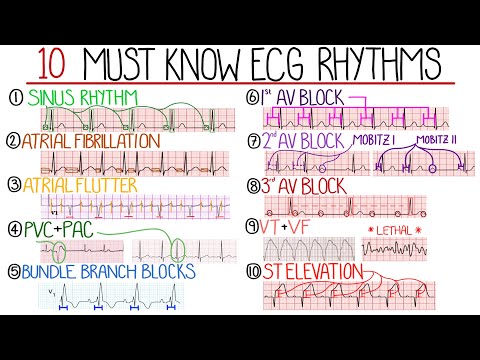
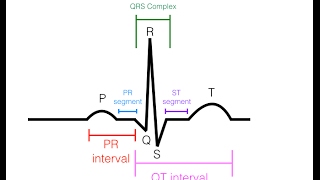
foreign [Music] we will look at some of the most common and must-know ECG findings in medicine we start with sinus rhythm the normal Rhythm of the heart in this instance there are regular p waves followed by a QRS complex that represents normal conduction of the electrical signals from the sinoatrial node in the right atrium through the atrioventricular node and bundle of hiss into the ventricles the PR interval which is the time between the start of the P wave and initiation of the QRS remains constant throughout the QRS complex itself represents ventricular depolarization and is normally
narrow typically between 80 and 100 milliseconds in adults if the rate is below 60 beats per minute this is sinus bradycardia and above 100 beats per minute is sinus tachycardia next we have atrial fibrillation in this case there is abnormal electrical activity that leads to the atrial muscle fibers Contracting at different times it is these uncoordinated contractions that give the quivering or fibrillating activity the ECG therefore has no clear p waves with QRS complexes not being preceded by a P wave although the fibrillations can somewhat resemble a P wave at times they will not be
consistent only some of the electrical signals get conducted down into the ventricles and therefore lead to ventricular depolarization but there's no real pattern of which impulses will get conducted therefore we end up with the textbook irregularly irregular heart rhythm this is described as a variable interval between the r waves on the ECG generally it occurs as a result of a substrate that will maintain the arrhythmia such as dilatation of the Atria and a triggering event such as electrical activity arising from another atrial location most commonly this is in the region of the pulmonary veins rates
above 100 beats per minute are known as atrial fibrillation with rapid ventricular response while those under 60 beats per minute are atrial fibrillation with slow ventricular response I have a video dedicated to atrial fibrillation and will leave a link to it atrial flutter is often mistaken for atrial fibrillation they are similar the main difference is that atrial flutter features coordinated electrical activity in the Atria due to a re-entry circuit leading to Rapid contraction of the Atria this is usually around 300 beats per minute with a regular atrial rate and narrow complex tachycardia as a useful
side note supraventricular tachycardia is an umbrella term to describe tachyarhmias With An Origin above the ventricles that's a classically described as narrow complex tachycardias examples include sinus and atrial tachycardia as well as atrial fibrillation with rapid ventricular response and atrial flutter amongst others the ECG in atrial flutter classically shows a Sawtooth pattern coming from inverted P waves usually in the inferior leads it is also described looking at the number of p waves compared to the number of ventricular contractions showing the ratio of non-conducted to conducted beats most commonly this is two to one giving a
ventricular rate around 150 beats per minute and higher ratios indicate a higher degree of block through the atrioventricular node the term block here is not the same as the AV blocks that are coming up it is worth noting that the conduction ratio of one to one is possible and is highly associated with instability and progression to ventricular fibrillation these ratios can be variable in the same patient making the ventricular rate irregular which is why it can often be mistaken for atrial fibrillation now we have premature contractions which are extremely common findings on ECGs premature ventricular
contractions or PVCs are Beats that originate from the histor kinji region of the conduction system and therefore appear as wide complex beats above 120 milliseconds in duration there is then a compensatory pause before the next beat although can be felt as palpitations they are rarely dangerous alone unless they are frequent defined as over 10 to 30 per hour and if happening every other beat are described as by Gemini while having a sequence of PVCs one after the other may be described as ventricular tachycardia which we'll cover later on premature atrial contractions or Pacs are seen
as a P wave with a different morphology to the regular sinus p waves followed then by a narrow QRS complex the beat following the PAC May resemble a pause however if you track out the expected location of the P wave it should fall at approximately the expected time Pacs do not typically require further investigation bundle branch blocks are another feature that are fairly common in general these are described as left or right bundle branch blocks it's worth knowing as well that the left bundle branch splits again into the anterior and posterior branches these patterns feature
wide QRS complexes Beyond 120 milliseconds left bundle branch blocks feature a deep S Wave in V1 and prolonged R wave in V6 giving a w and m shape respectively while right bundle branch blocks have an rsr wave pattern in V1 and prolonged S Wave in V6 giving M and W shapes respectively an easy way to remember this is with the mnemonic William marrow also remember that the ST segment is affected in bundle branch blocks and so interpreting St changes is challenging and needs specific criteria now let's take a look at the atrioventricular or AV blocks
first degree AV block is due to slowed conduction through the AV node shown by a prolongation of the PR interval Beyond 200 milliseconds in general this is a fairly benign finding but can in some instances progress to higher degree blocks second degree AV block has two main types called mobit 1 or wenkebach and mobitz 2 or hey mobit 1 features a progressive lengthening of the PR interval until there is a non-conducted P wave then the cycle repeats mobits 2 features a non-conducted P wave with no variation in the PR interval type 2 is usually due
to a structural abnormality and is considered high risk for progression to third degree also known as complete heart block in third degree AV block there is no association between atrial and ventricular contractions on the ECG this appears as p waves that do not lead to a QRS complex and more p waves than QRS complexes indicating a higher atrial rate than ventricular rate which is most commonly severely bradycardic typically there are regular POS waves and regular QRS complexes but no association between the two with the QRS complexes being generated by junctional or Escape rhythms I also
have a video dedicated to Heart blocks that are link here next we have ventricular tachycardia and ventricular fibrillation which are two crucial ECGs to recognize ventricular tachycardia is defined as a broad complex regular tachycardia the main type being monomorphic ventricular tachycardia where there is a single source for the beets and so the QRS complexes in one lead all look the same polymorphic VT is the term used when there is more than one source of the ventricular beats and so gives varying morphologies of the QRS complexes one famous example of polymorphic VT is torsades the points
occurring in the setting of a prolonged QT interval although other causes for regular broad complex tachycardia exist it isn't straightforward to distinguish them and generally if there is any diagnostic uncertainty it is treated as ventricular tachycardia some features suggesting VT include very broad complexes above 160 milliseconds absence of bundle branch block morphologies and the presence of extreme axis deviation ventricular tachycardia itself can result in Cardiac Arrest but may also degenerate interventricular fibrillation which is a lethal Rhythm if not treated there are no clear p waves or QRS complexes and therefore minimal cardiac output the ECG
features chaotic electrical activity of varying amplitudes with the amplitude correlating to duration as time goes on it reduces until asystole is reached these two arrhythmias are associated with Cardiac Arrest defined as cessation of normal blood circulation due to failure of the heart to pump blood and are the two shockable rhythms in Cardiac Arrest The non-shockable rhythms being pulseless electrical activity and asystole number 10 is one of the most famous ECG abnormalities St elevation although not in arrhythmia it is an important ECG feature on the ECG this is the portion between the end of the S
Wave and the beginning of the T wave acute myocardial infarction is largely the most significant cause however there can be many other causes too including pericarditis left bundle branch block left ventricular hypertrophy and even a normal finding such as in benign early repolarization typically the elevation is defined as more than one millimeter from the isoelectric Baseline in any lead apart from Leeds V2 and V3 that generally require at least 1.5 millimeters also remember that different leads represent different territories of the heart leads 1 AVL V5 and V6 are lateral leads 2 3 and avf are
inferior well V1 to V4 are anterior and septal for a posterior view additional chest leads V7 to v9 are needed in stemi you expect the elevation to be present in territories that are affected by the blocked coronary artery and St depressions in opposite territories termed reciprocal changes which is why if St depressions are seen in the anterior leads an ECG with leads V7 to v9 should be done which may reveal posterior stemi check out my video specifically on ECG interpretation and I recommend sources like Life in the Fast Lane and ECG waves for further reading
which are the main references for this video
Related Videos
8:59
Understanding Sepsis (Sepsis Explained Cle...
Rhesus Medicine
457,971 views

48:44
EKG Rhythms | ECG Heart Rhythms Explained ...
RegisteredNurseRN
793,848 views

13:08
ECG Interpretation Made Easy (Learn How to...
Rhesus Medicine
962,045 views

17:46
Heart Conduction System & ECG (EKG)
Siebert Science
80,948 views

18:31
Understanding Arrhythmias
Zero To Finals
65,591 views
18:26
ACLS Practice Test with Answers - Pass the...
Florida Training Academy
114,381 views

22:50
EKG/ECG Interpretation Basics Nursing NCLE...
RegisteredNurseRN
1,002,484 views

1:19:14
EKG Basics | How to Read & Interpret EKGs:...
Ninja Nerd
2,584,547 views
12:24
EKG/ECG Interpretation (Basic) : Easy and ...
MINT Nursing
6,209,687 views

14:05
Common ECG abnormalities | MADE EASY!
Medicine Made Simple
115,619 views

38:08
ECG (EKG), Sinus rhythm and abnormalities
Dr. John Campbell
374,345 views
13:09
Are You A Medical Legend? Test Your Knowle...
The Learn Medicine Show
43,120 views

9:22
Autism Spectrum Disorder Explained Clearly...
Rhesus Medicine
134,505 views

40:50
Cardiac dysrhythmias (arrhythmias) (common)
Dr Matt & Dr Mike
147,019 views

40:13
#ecg interpretation : The animated Visual ...
The Learn Medicine Show
48,387 views
11:04
EKG Rhythms | Top Tested NCLEX Review | Ho...
SimpleNursing
744,351 views

6:56
EKG like a BOSS Part 1 - How to Read EKGs ...
NURSINGcom w/Jon Haws, RN
1,259,256 views

26:57
ECG Interpretation Made Easy; How to read ...
MedNerd - Dr. Waqas Fazal
624,388 views

18:51
Basic Arrhythmias | Sinus, Brady, Tachy, P...
ICU Advantage
572,559 views

20:44
How to Read an ECG | ECG Interpretation | ...
Geeky Medics
300,011 views