The Cardiovascular Exam / Heart Sounds (Strong Exam)
19.97k views7119 WordsCopy TextShare

Strong Medicine
A deep dive on the "core" cardiovascular exam - the exam of the heart and blood vessels that one wou...
Video Transcript:
[Music] hello in this video I'll be doing a deep dive on the core cardiovascular exam with a demonstration of specific Maneuvers as well as a discussion of common pathologic findings and how to document those findings in the medical record consistent with this physical exam series The Core exam includes both screening Maneuvers to detect asymptomatic disease as well as General Diagnostic Maneuvers with an emphasis on those that are supported by evidence in the primary literature along with the neuro exam the cardiovascular exam is particularly nuanced and provides a rich window to logically connect observed findings with
the underlying path of physiology radica here will be helping out uh today with our demonstration but to start us off I'll spend a minute reviewing cardiovascular Anatomy as it relates to surface landmarks so here's the Torso let's visualize where the rib cage lies and the heart and great vessels beneath it when describing the location of findings in the cardiac exam we need to refer to the surface landmarks because that will be a point of consistency between exams performed at different times or by different people most of these landmarks are relatively obvious for example the ribs
the intercostal spaces between the ribs the sternum and the clavicles the sternum is subdivided into three sections the upper manubrium the body and the much smaller zpid process the single most important Landmark for the cardiovascular exam is the sternal angle which is the near motionless joint between the manubrium and the body of the sternum which is a subtle but palpable landmark in most individuals the sternal angle is also a occasionally known by the eponym angle of Louie or even angle of Lewis now you might assume that angle of Lewis is a result of Americans just
butchering French names but in reality the source of the eponym is not completely certain so we really don't know how to pronounce it properly which is just another reason to call this the sternal angle there are two major reasons why the sternal angle is so important first it's location of the junction of the second rib with the sternum which then allows you to identify the number of every other rib by just walking your fingers down the chest wall the second reason is because there are several critical anatomic structures beneath this Landmark most notably the aortic
Arch the tracheal bifurcation and the pulmonary trunk there are also several imaginary lines on the chest wall the mid sternal the midclavicular anterior axillary and mid axillary lines together the imaginary anatomic lines and the very real ribs and intercostal spaces create a grid that's used for localization so for example I could say that I heard a particular extra heart sound best in the left midclavicular line in the fifth intercostal space which also happens to be a typical location of the cardiac Apex in healthy individuals there are also paired lateral sternal and parasal lines but these
terms are rarely used in clinical practice unlike the pulmonary and abdominal exams which are typically performed in one position each the core cardiovascular exam is usually performed with a patient in multiple positions we'll begin with the patient see the upright and fully covered one might reasonably consider assessment of the pulse rate and blood pressure as a part of the cardiovascular exam though in most clinical scenarios these will have already been measured by by a nurse or medical assistant in this series I cover the assessment of the vital signs in a separate video from here I
think it's best to start with assessment of the patient's pulse there are different opinions on which pulses to check in which patients for an exam in a younger healthy asymptomatic patient I would check just one radio pulse only assuming the rest of the exam was also unremarkable but even that might be reasonably skipped whereas in a middle-aged or older patient or in a younger patient with significant cardiovascular risk factors I would also check both the posterior tibial and dcals pedus pulses given the possibility of picking up peripheral vascular disease but because it's more efficient to
talk about all the pulses at once I'll demonstrate the location and palpation of each one now here's the location of the radial artery on the flexor surface of the lateral wrist it's recommended to use your second second and third fingers rather than your thumb to prevent you from mistaking your own relatively prominent thumb pulse for the patient's pulse the brachial pulse is most easily felt by finding the biceps tendon in the anticubital FASA and palpating about 2 cm medial and 2 cm proximal it requires more pressure from your fingers to feel this than the radial
pulse did moving to the leg the doalos pedis pulse can most often be felt in the midfoot just lateral to the extensor tendon of the great toe but there is some variability here and you may need to feel round for it for hospitalized patients with vascular issues you sometimes see a little X drawn in pen on top of each foot denoting where this pulse has been previously found to make serial examinations easier moving to the rear of the foot the posterior tibial pulse is just behind and slightly below the medial malleolus of the ankle it's
not uncommon common for a healthy patient to have either a non-p palpable dral pedus pulse or a non-p palpable posterior Tubi pulse but it's rare for a healthy patient to have neither of these palpation of the palal pulse can be done in the sitting position though it's easier when the patient is supine have the patient Flex their knee to make an angle of around 150° or so reach around under the knee and place both sets of your second and third fingers together right in the middle of the poil fossa then have the patient fully relax
their leg in that flexed position I like using the phrase let your leg sink down into my hands palpation of the femoral pulse is not often indicated but is performed in the sepine patient by placing your fingers just distal to the ingal ligament midway between the anterior superior iliac spine and the pubic symphysis because of its location you want to be particularly clear with telling your patient what you are about to do while it's generally frowned upon to examine part of the body that's not been visibly exposed this is a time in which I personally
think it's actually okay last is the cored arteries these can be examined either with the patient sitting supine or anywhere in between palpate the corage just medial to the sternal cleidomastoid muscle at about the level of the cord cartilage avoid pressing at the level of the thyroid cartilage since this is the location of the kateed sin and pressure there may result in the patient passing out also do not palpate both creds at the same time for the same reason now that you know where all the arteries are located what specifically are we assessing them for
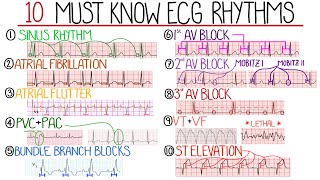
two things the first is the pulses regularity which you only need to assess once the second is each pulse's strength if the pulse is irregular try to determine if it's regularly irregular meaning there's a fixed pattern to the pulse there are specific arrhythmias that display this specific pattern for example type 1 second degree a block as well as something called biny and trigeminy it's okay if you're not yet familiar with those rhythms from ECG interpretation alternatively the pulse may be irregularly irregular meaning that there is no pattern that it feels random that's what's seen with
atrial fibrillation and atrial flutter with variable blocks there's a third abnormal pattern though that can be easily mistaken for irregularly irregular which is regular with occasional early or missed beats this is what's seen with sinus rhythm plus intermittent premature atrial or ventricular contractions the reasons that some pulse beats are missing rather than all of them occurring early is because sometimes the premature beats are so early that diastolic filling has not yet occurred and so there is minimal forward blood flow that's generated by that particular ventricular contraction regarding the pulse strength along the way during your
training you'll likely be taught a numerical scale that assigns the strength of a pulse a number from 0 to 4 plus however there is not sufficient consensus as to what these numbers actually mean therefore to reduce ambiguity and minimize miscommunication I recommend using a single word descriptor instead of a number for example describing each pulse as either absent diminished normal or bounding meaning greater than normal on occasion a clinician may also use the term non-p palpable but dopplerable meaning that even though they could not feel the pulse when they used a Doppler ultrasound at the
bedside they were able to demonstrate that the vessel still has blood moving through it a diminished pulse and in particular an absent one should prompt The Examiner to assess the relative temperature of the extremities to see if the one without a pulse is cooler than the other side it should also prompt The Examiner to assess the next most proximal pulse in that extremity so for example if the radial pulse is not palpable you would next attempt to palpate the brachial pulse on that side on the other hand if the radial pulse is normal or bounding
it's unnecessary to palpate the ipsilateral brachial ideologies of absent or diminished pulses can be separated into focal versus generalized a focal decrease particularly in the legs suggests atherosclerosis rare causes include an embolis an arterial dissection in which the layers of the wall of a large muscular arteries start to peel apart from one another or vasculitis which is autoimmune mediated inflammation of the blood vessels a generalized decrease in all pulses can be seen with low cardiac output either from heart failure or hypovolemic shock as well as with aortic stenosis bounding pulses are always generalized and suggest
either aortic regurgitation or a hyperadrenergic state such as sepsis drug intoxication or withdraw and hyperthyroidism as a general rule if a patient's pulses are all symmetric the subjectively perceived strength of them is proportional to the objectively measured pulse pressure which is the difference between the systolic and the diastolic blood pressures now let's talk evidence in the diagnosis of peripheral vascular disease of the legs an asymmetrically cool leg or an absence of both oralis pedus and posterior tibial pulses substantially increase the probability of PVD while the lack of these findings have a modest influence on rolling
it out at the same time as pulse Assessments in the legs you you can also assess for peripheral edema or swelling while edema can be generalized to the whole body affecting all four Limbs and even the Torso in that case the ideology is almost always low serum albumin and is not directly related to the cardiovascular system edema of the legs is primarily assessed by holding firm pressure to either the feet or shins and seeing if the pressure of your finger pushes subcutaneous fluid out of the way and allows your finger to SN down into the
patient soft tissue if a patient has EMA you should characterize it based on whether it's unilateral or bilateral and if bilateral whether it's symmetric describe how far up the leg it extends and also describe it as either pitting or non-pitting in which pitting edema is that in which an indentation transiently remains in the patient's skin even after you remove pressure from your finger as with the pulses there is a fourpoint numerical scale that is used to grade the severity of Edema but also as with the pulses and even more so there's actually no consensus on
what the scale actually means does it refer to how far the edema pits in how far up the leg it extends or how long it takes for the pitting to resolve after the pressure is released I've heard all these over the years and yet virtually no formal physical exam reference mentions any of them so despite its near ubiquitous use in practice I actually Rec recommend avoiding use of the 4o Dema scale and instead you should describe EMA with General words like mild moderate and severe which you know are equally vague but don't falsely imply agreement
on definitions which the scale does or alternatively describe the diema very specifically if it's a central feature of the patient's presentation ideologies of pitting edema are many just the relatively common ones include heart failure curosis renal failure malnutrition deep vein thrombosis cellulitis chronic venostasis pregnancy and a medication side effect because of the high number and the diversity of the different causes of pitting edema its presence is usually of minimal diagnostic utility and identifying it is more helpful to understand the manifestations of a disease diagnosed via other means using the presence of penting EMA as the
primary argument that a patient has intravascular volume overload for example is a very common mistake on the other hand non- pining edema is much less common and suggests lymph edema which is a general term for edema that's caused by blockage of the limb's lymphatic drainage due to tumor radiation Sur surgery or infection including recurrent episodes of cellulitis there's also a condition called lipedema which resembles lymphodema but instead of an accumulation of fluid It's actually an accumulation of adapost tissue in the legs lipedema can be distinguished from TR adeema because it spares the feet the next
maneuver I'll be discussing is assessment of the jugler Venus pressure or jvp while interpreting jvp isn't as complex as interpreting cardiac oscilation it seems to elicit a disproportionate share of frustration among trainees in short the jvp is a surrogate for the central Venus pressure or CVP in the right atrium abnormalities of the jvp either the overall pressure or abnormal patterns in the pressure that's seen across the cardiovascular and respiratory Cycles provide helpful information that's relevant to almost any cardiac condition because it's so important and because it's so confusing I'll spend a little extra time here
with the explanation of how this physical exam finding works as well as its limitations since the jugular vein is directly connected to the right atrium via the superior vnea and the jugular vein is a highly compliant vessel meaning that it readily dilates when filled with blood but collapses when it's empty we can estimate the CVP by examining how high the jugler veins distension extends in other words we use the internal jugular vein as a blood-filled monometer for example suppose a patient is fully upright at 90° and the jugular Venus pressure extends to this level we
can say that the central Venus pressure is proportional to the vertical distance between that level and the level of the right atrium and to simplify units we use units of centimeters of water using the fact that the density of blood and water are approximately the same but how do we know where the right atrium is clinicians make an assumption based on an old observation that the right atrium tends to sit approximately 5 cm closer to the ground than the palpable sternal angle so one can therefore determine the central Venus pressure in units of centimeters of
water as the sum of the height of the jvp above the sternal angle and 5 cm in those patients who are unable to sit fully upright the method stays the same it doesn't matter what the angle is that the patient is at all that matters is the vertical distance to which the jugular vein's distension extends though this requires the assumption that the right atrium will still be 5 cm closer to the ground than the sternal angle irrespective of what angle the patient is at however in practice there are limitations to precisely measuring CVP with this
technique for example one needs to be able to distinguish Venus from arterial pulsations and in patients of larger body habitus the jugular vein May simply not be visible at all there are also physiologic limitations measuring hydrostatic pressure which is what we're doing by definition requires the fluid to be stationary which of course is not true of the blood of the jugular vein as we can see the jbp oscillates with one period synchronized with the cardiac cycle and another synchronized with a respiratory cycle in the cath lab where there's a catheter that's directly transducing the pressure
in the right atrium the CVP is measured at end expiration but in 20 years as a physician I have yet to see a clinician at the bedside deliberately time their jvp measurement to the respiratory cycle even the sacrosanct 5 cm that's added to the jvp is an oversimplification the assumption is that the right atrium is always 5 cm below the sternal angle irrespective of inclination of the patient torso and irrespective of the size of the patient is just not true the original descriptions of this method in a 1946 paper is Illuminating the authors openly adopted
the 5 cm number for Simplicity and they acknowledged the uncertainties and potential sources of error which many modern physical exam references seem to have forgotten so conceptually this is a valid technique to estimate the CVP as as long as one realizes there is a significant range of error all these reasons are why I think attempts by Old School exam gurus to use a ruler and straight edge to precisely measure the jvp to the nearest centimeter are misguided and I wish we would stop teaching students to do this instead here's a practical approach to the jvp
unless you have a strong suspicion that the patient's jvp will be unusually high or unusually low I recommend starting with a patient at either 30 or 40 5° their head and neck should be relaxed and without a pillow conventionally the right I J is used to estimate the jbp because the waveforms are easier to see as compared to the left and it's examined from the patient's right side there is a difference of opinion on whether the head should be turned or in a neutral position turning the head away from the side being examined is far
more common but a plausible argument suggests that this stretches the fascia and muscles across the veins obscuring them more I tend to split the difference between these opinions and have the patient very modestly turn their head to the left a tight directed light shown tangentially across the neck will cast Shadows making the waveforms much easier to see if the room is unusually bright you might even consider dimming it slightly for this part of the exam by drawing the blinds or turning off the overhead light the internal jugular vein lies deep to the external clom mastoid
muscle and unlike the external jugular vein cannot be directly seen however the pulsations from the vein are transmitted through the muscle to the overlying skin the jvp is then typically measured as the highest point of oscillation through the respiratory and cardiac Cycles if you cannot see the pulsations it may be because the jvp is higher or lower than you anticipated in which case you may need to raise or lower the patient to a different angle in short the best angle at which to examine the jvp is the one in which the jvp is easiest to
see so that happens to be 30 to 45° in patients with normal intracardiac pressures I'd like to come back to one of the aformentioned limitations of jvp measurement how to differentiate the jugular and kateed pulsations which can be a real challenge with some patients nexts if you're having difficulty with this which is common consider the following characteristics Venus waveforms in healthy individuals have two undulations per cardiac cycle whereas the cored waveform has just one with Venus waveforms there's typically a slower movement out and then a more rapid movement in whereas with a cored waveform it's
typically more rapid out and gradual back in Venus waveforms are usually not palpable whereas ceds are Venus waveforms usually fall during inspiration whereas there is no effect on the catds and the external application of pressure to the abdomen causes Venus waveforms to transiently rise whereas the cids are once again unaffected in some patients pulsations within the internal jugular vein are not visible at all but the external jugular vein which is superficial to the sternal clom mastoid is visible in most cases using the external jugular vein to estimate CVP is fine though the specific waveforms may
be less prominent a normal jvp is 8 cm of water or less which is roughly equivalent to being able to just barely see it above the clavicle in a patient at 45 to 60° as implied earlier it's my opinion that measuring jvp to a specific value is neither precise nor accurate and it is thus a waste of time instead I qualitatively characterize jvp as being normal elevated or in some uncommon cases extremely elevated there are some instructors who teach that in unusually low jvp is indicative of hypovolemia but differentiating between normal and low jvp is
difficult the cut off between the two appears arbitrary and the primary literature makes virtually no mention of this finding so I don't think low jvp is a diagnostically helpful finding to look for likewise I would avoid the term flat jvp which is ambiguous as to whether one is implying it's normal or is implying that it's much lower than normal or in some cases The Examiner May simply not have seen the jvp at all and is just assuming that's because its value is so low which is an assumption that can easily be incorrect among patients suspected
of elevated CVP the jvp has consistently been found to be a good surrogate for Central Venus pressure as directly measured by catheter though if you do attempt to measure a specific for the jvp it may systematically underestimate the pressure by a few centim of water and if comparing the observed jvp to CVP is measured via a central line or something in the cath lab remember that the CVP is usually measured and reported in units of millimeters of mercury not centim of water so you need to convert between the two the causes of an elevated jvp
are many but most notably all forms of heart failure pulmonary hypertension a large pulmonary embolism and cardiac tamponade an important point of which most non-critical care docs are unaware there's a difference between saying that this jvp is a good surrogate for CVP and that the jvp is a good surrogate for determining fluid or diuretic responsiveness a discussion of this distinction is outside the scope of this video but in extreme brief the jvp is more helpful for diagnosis than it is for guiding management there's also a relevant anonomous finding called kousal sign which is a paradoxical
increase in the jvp during inspiration this finding is classically described in constrictive paric carditis but it can be observed in any cause of severe right heart failure in addition to determining whether or not the patient's jvp is elevated you also want to observe these specific waveforms as mentioned earlier the normal Venus waveform has two undulations per cardiac cycle the first outward movement occurs immediately before S1 this is known as the a-wave which is caused by atrial contraction it's followed by the X descent then the v-wave occurs around S2 followed by the Y descent what are
some abnormalities that can be seen in the waveforms Canon a waves which are the intermittent occurrence of a very prominent outward wave CA by the Atria Contracting against an already contracted ventricle is seen in AB dissociation in patients with severe trusper gradutation they have a giant outward wave that occurs during syy that makes the A and V waves seem connected and absent a waves suggest a lack of atrial contraction as seen in either atrial fibrillation or sinus arrest with a junctional or ventricular Escape Rhythm a number of other waveform abnormalities are described but they're difficult
to identify without a printed tracing of the directly transduced pressure from the cath lab next let's discuss listening for kateed brewes a brew is the name given to the whooshing sound that's generated by turbulent blood flow through a vessel brewes are most classically associated with atherosclerotic narrowing of an artery though it's been reported that 1% of normal adults have them Kate brewes are always louder insistently if you hear what sounds like a brewery in the neck but it's louder in diam Hy it's likely turbulent flow through an internal jugular or brachio spalc vein known as
a Venus hum which is a benign phenomenon occasionally observed in healthy individuals to listen for a kateed brewey place your stethoscope in a region under the angle of the jaw anterior to the sternal clom mastoid muscle and superior to the level of the thyroid cartilage notably this is a little bit above the exact point where the crowed pulse is best palpated here's what a brewery would sound like so what's the evidence for kateed oscilation a brew substantially increases the likelihood of a clinically significant cenosis and its absence modestly decreases the likelihood notably other arteries in
the body can also get brewes for example I discussed Reno artery brewes in the core abdominal exam video in addition to this if any extremity is noted to have a diminished pulse that artery should also be osculated since the presence of a brewey will further increase the probability of peripheral vascular disease in that limb the final maneuver to discuss within the core cardiovascular exam is oscilation of the heart while it's a very simple maneuver to perform the interpretation of observed abnormalities are the most complicated asp ECT of the entire head to toe physical exam with
the debatable exception of some cognitive tests osculation is classically performed with a patient between 30 and 45° though it's also fine to be done with the patient supine some references recommend listening to the patient in three locations upright Supine and left lateral decubitus though I've never seen that done in actual practice there are four to five classic locations to listen to the heart the first four roughly correspond to being directly above the four valves thus these are often referred to as the aortic pulmonic tricuspid and mitro areas however I strongly recommend not referring to them
as such since the surface location over which a particular sound is best heard does not always sit above the valve responsible for making that sound so instead refer to the location by surface landmarks these second right intercostal space just lateral to the sternum the second left intercostal space also just lateral to the sternum the fourth left intercostal space also just lateral to the sternum and the fifth intercostal space in the midclavicular line which actually sits more over the apex of the heart than over the mitro valve anyway the optional fifth location for osculation is located
in the left third intercostal space and is known by the eponym of herb Point whether oscilation at this fifth location is necessary is a matter of opinion and personal preference I tend to not listen there unless I'm trying to better understand an abnormality I've already heard in either of the adjacent intercostal spaces for a patient without breasts this exam can be performed with the front of the Gown lower to the waist however for a patient with breasts we want to expose only what's necessary thus for oscilation at the upper two spots ask the patient to
lower the Gown to the upper breast and then for oscilation at the lower two spots ask the patient to raise the top of their gown back to the shoulders and raise the bottom of the Gown to just under the breasts you may also need to ask the patient to hold their left breast up and out of the way to make it easier to osculate at the cardiac Apex do not move the patient's breast yourself and do not listen to the Apex through the breast some practical guidance on oscilation and gowning and draping first while generally
you want to expose whatever part of the body you are examining depending on what the patient is wearing and their comfort level you may choose to reach under the Gown to osculate in the proper location depending on the context this may be okay to do provided that you let the patient know what you'll be doing immediately beforehand second if instead of a gown the patient is wearing an article of clothing that simply isn't conducive to being raised and lowered in the same manner and if changing into a gown is Not Practical as long as the
material is thin it is not a catastrophe to listen through the clothing given that the sound is already traveling through several centimeters of muscle and soft tissue an extra 1 to 2 mm of cotton doesn't make a huge difference again it's definitely not preferable to osculate through clothing but it is better to do so than to not osculate at all conventional teaching is that the wider and shallower diaphragm of the stethoscope head should be used for this because it better transmits higher pitch sounds which most cardiac sounds and murmurs are and then the deeper and
coverless Bell of the stethoscope is additionally used at the cardiac Apex to listen for three specific low pitch sounds that can occur at that location however after spending years using many different models of stethoscope I found that the difference in sound between the diaphragm and the bell of a conventional acoustic stethoscope to be so small as to not make a significant difference however for those with access to a digital stethoscope that can apply a digital filter to selectively amplify some frequencies more than others that does make a big difference when listening to the heart sounds
particularly for trainees it may be best to focus on just one particular aspect of what you're hearing at a time so for example first just try to figure out the location of syy versus diast for patients with a normal heart rate this can be done by remembering that syy is shorter than diast however as the heart rate is uh increases diasy shortens more than cyly thus once the heart rate exceeds around 120 beats per minute or so cyly and asly may be close enough in duration that it can be very very difficult if not impossible
to determine which is which just from sound alone in which case simultaneously feeling for the patient's pulse may be helpful also don't be shy about taking your time with oscilation it's by my it's been my observation that the most common reason an examiner misses a murmur or extra heart sound is because they rushed listening for it in a normal patient there should be two relatively Sharp heart sounds called S1 and S2 for the first and second heart sound S1 comes at the transition from diast to syy and is generated by the simultaneous closing of the
mitro ENT tricuspid valves S2 comes at the transition from syy to diast and is generated by the simultaneous closing of the aortic and pulmonic valves as a general rule S1 is best heard at one of the lower two oscilation positions while S2 is best heard at the upper two oscilation positions but both should be easily heard in all locations and together the S1 and S2 comprise the ldub of the heart well S1 is normally a single sound throughout the respiratory cycle S2 normally displays a phenomenon called physiologic splitting in which it is a single sound
during expiration and becomes a very subtle double sound during inspiration this is due to the aortic valve closing slightly earlier during inspiration and the ponic valve closing slightly later when the two components of S2 can be distinguished from one another the aortic component is known as A2 and the ponic component is P2 to determine that the degree of split is normal and not excessive of it requires a lot of practice but in short a normal physiologic split S2 is just barely perceptible by most examiners regarding possible abnormalities that can be heard it is an incredibly
complex topic that is a focus of an entirely separate video of its own but here's a summary of how these abnormal sounds can be characterized there can be abnormalities of normal sounds such as an abnormally loud or soft S1 or variably loud S1 a loud P2 suggesting pulmonary hypertension mechanical sounding S1 or S2 caused by a mechanical valve replacement or a variety of abnormal S2 splitting there can be abnormal sounds that should not be there at all the classic examples in this category are the so-called third and fourth heart sounds better known as S3 which
occurs in early diast and S4 which occurs in late diast and corresponds to the atrial kick S3 and S4 are distinct sounds in that they are both relatively low pitched compared to S1 and S2 together S3 and S4 are also known as gallops other less common abnormal sounds include an aortic ejection click in very early syy the click of a mitro valve prolapse in mid syy and the so-called opening snap of mitro stenosis in early diast then distinct from heart sounds are heart murmurs heart murmurs are like brewes longer duration acoustical phenomena caused by turbulent
blood flow they are classically subdivided based on timing whether they occur during syy such as that from aortic stenosis mitro regurgitation or in Pediatrics a ventricular sepal defect or occur during diast such as aortic of regurgitation and mitro stenosis other valvular diseases can also cause murmurs but these are collectively uncommon to hear if you do hear a murmur in addition to its timing there are other characteristics which you should describe the location where it's best heard the intensity which is typically graded on a 1 to scale in the 21st century it has become very rare
to hear a murmur louder than a three out of six on that scale describe the shape of the murmur meaning how does it change over its duration which provides a clue to its cause for example here's a classic systolic Crescendo de Crescendo murmur of aortic stenosis and here is the classic holosystolic or uniform murmur of mitro regurgitation and the classic de Crescendo diastolic murmur of aortic regurgitation describe if the murmur radiates to anywhere meaning is there a place other than directly over the heart where the murmur is heard award ex stenosis murmurs can radiate to
the coted arteries where they might sound like a cored brewery mitro regurgitation murmurs classically radiate towards the left axilla in short murmurs tend to radiate in the direction that the turbulent blood is Flowing some clinicians will also describe the pitch of the murmur and the subjective character of the murmur such as harsh or musical or blowing this becomes a bit more advanced but finally murmur can also be characterized based on how their intensity or timing change with physical Maneuvers that the patient does for example what effect does deep inspiration isometric hand grip a Val Sala
maneuver or sudden standing have on the murmur all of which can provide information about the underlying pathology there are two specific murmur terms that are frequently misused the first is a flow murmur this is a murmur caused by Blood moving through a physically normal valve in which the turbulence is caused by either low viscosity of blood from anemia or a high velocity of blood in states of catac colomine excess such as sepsis the second misused term is an ejection murmur which is a systolic Crescendo de Crescendo murmur heard at the upper sternal borders caused by
Blood moving forward through the aortic or less commonly pulmonic valve I find this latter term to be vague some clinicians use it to describe any systolic cresendo decrescendo murmur While others specifically use it for early murmurs that is systolic murmurs that do not extend all the way to S2 for some clinicians the term implies in ideology other than aortic stenosis While others routinely refer to the murmur from AIC stenosis as an ejection murmur so in short flow murmur is fine if used correctly but I would avoid the term ejection murmur since you don't know if
the listener or reader has the same understanding of the term as you do as mentioned if you want a more in-depth discussion of cardiac oscilation there is a separate video that does an even deeper dive on this when it comes to the evidence behind cardiac oscitation I'm only going to focus on a couple of key findings to remember but there are many more in the literature an absent or soft S2 in a patient who concurrently has a systolic Crescendo de Crescendo murmur increases the likelihood of aortic stenosis although it's frequently taught and is my personal
experience that a loud S2 is suggestive of pulmonary hypertension this has not yet been shown in the literature the presence or absence of an S3 is helpful at identifying or ruling out a reduced ejection fraction however neither the presence nor absence of an S4 is helpful in determining whether a patient has elevated left sident filling pressure this surprises a lot of people because the S4 is frequently taught to be a sign of diol dysfunction but in fact it's more or less a useless finding whose primary significance is that it can be mistaken for something else
or vice versa whether or not the examiner Hears A characteristic murmur of aortic stenosis iic regurgitation or mitosis all will have significant impact on the presence or absence of those vular diseases and here the meaning of characteristic quote unquote refers to a combination of classic timing shape and location I'll end with the discussion of the documentation of the cardiovascular exam as with the exam as a whole there is more Nuance here than with the documentation of other exam components inspection is not typically included in documenting the CV exam and instead by convention in the US
documentation of a normal exam starts with rrr for regular rate and Rhythm I'm not a huge fan of this terminology as I'm not sure what a regular rate even means if it just means a normal rate well that would already have been documented under the vitals I think just regular rhythm is fine F though you may hear some old school Physicians object to this as well saying that a regular rhythm can only be determined with an ECG and that regular pulse is the more accurate description but this seems excessively pedantic it's conventional to follow this
with normal S1 and S2 though be careful to not misapply this phrasing for example saying that S2 is normal implies the existence of a physiologically split S2 during inspiration if there is no S2 split then I would instead document normal S1 absent S2 split next clinicians will frequently write no m r or G for no murmurs rubs or gallops this phrasing also has seemed strange to me since pericardial rubs are rare and we don't make a habit of routinely mentioning the absence of any of the other hundreds of equally rare findings we might conceivably encounter
on the exam I think no murmurs or galops is fine but no murmurs rubs or gallops is much more common if a patient has a murmur be sure to describe it as already reviewed its intensity timing shape location and radiation most often in that order and remember that intensity is actually the least important murmur characteristic despite it being the one most likely for the clinician to include some clinicians document the kateed oscilation and jvp assessment in a section for the neck where it's grouped with the assessment of the thyroid gland now I understand the logic
with that and it's not unreasonable I personally prefer to mention these in the CV section kateed brues are either present or absent and if present be sure to include which side for jvp as previously discussed many exam experts recommend providing a specific number in units of centimeters of water you know this is fine I guess some clinicians typically cardiologists are really attached to it and on the Ws you have to pick your battles but also as discussed bedside estimates of jvp have a lot of limitations so I think it's not only okay but maybe even
preferable to Simply State a jvp normal elevated or extremely elevated or alternatively mention its elevation in reference to a landmark such as elevated to the angle of the jaw with the patient fully upright if the jvp is not visible at the angles at which you examine the patient state that and mention the angle do not simply say no jvp uh or jvp flat then pulses as I mentioned earlier I recommend avoiding a numerical scale here and instead labeling pulses as absent diminished normal or bounding and last discuss edema also avoiding the extremely vague numerical edema
scale if the edema is a small part of the overall clinical picture it's okay to qualitatively describe it as mild moderate or severe with reference to how proximately the edema extends and instead if the edema is a significant part of the overall clinical picture such as the patient's Chief complaint consider objectively measuring limb circumference at a specific reproducible level such as the mid Shin that concludes this in-depth discussion of the core cardiovascular exam I'd like to thank radica for her assistance today and also be sure to check out the core cardiovascular exam without commentary to
see the flow of Maneuvers in practice as well as another video that covers a few specialized maneuvers [Music]
Related Videos

30:43
The Pulmonary Exam / Lung Sounds (Strong E...
Strong Medicine
22,562 views

36:33
Cardiac Examination Deep Dive - Clinical S...
Dr James Gill
370,213 views

18:11
The Cardiovascular Exam - Pulsus Paradoxus...
Strong Medicine
8,646 views

7:01
Heart sounds for beginners 🔥 🔥 🔥 S1, S2...
The Learn Medicine Show
1,392,645 views

1:20:36
Evolution of Cardiac Diagnostics: A New Er...
Dr. Pradip Jamnadas, MD
509,348 views

10:58
Learn Heart Murmurs In 10 Minutes (With He...
Rhesus Medicine
272,839 views

48:10
Cardiovascular Physiology - Pressure-Volum...
Medicosis Perfectionalis
122,113 views

12:49
Cardiovascular Examination - Explanation
University of Leicester
884,884 views
8:05
Cardiovascular Examination | OSCE Guide | ...
Geeky Medics
3,657,915 views

1:19:14
EKG Basics | How to Read & Interpret EKGs:...
Ninja Nerd
2,546,753 views

3:11:52
Diagnosis of SVT in the EP lab
Dr. Joshua Cooper - Arrhythmia Education
96,214 views

25:40
Living With A Pacemaker (common questions ...
Dr. Joshua Cooper - Arrhythmia Education
30,198 views
12:14
Most Common ECG Patterns You Should Know
Rhesus Medicine
1,496,732 views

43:59
Heart Sounds & Murmurs | Clinical Medicine
Ninja Nerd
103,532 views

18:31
Understanding Arrhythmias
Zero To Finals
49,238 views

8:24
Cardiac Examination (OLD VERSION) - Clinic...
Dr James Gill
627,613 views

12:55
Macleod's examination of the cardiovascula...
Farsight Channel
2,229,366 views

10:57
Respiratory Examination - Clinical Skills
Oxford Medical Education
435,777 views

20:11
The Full Neurological Examination
UCL Clinical Skills
723,389 views

7:13
Cardiovascular Exam Demo (Strong Exam)
Strong Medicine
10,293 views