ECG Interpretation | Clinical Medicine
302.07k views6499 WordsCopy TextShare

Ninja Nerd
Exclusive USMLE Step 2/PANCE Lecture… for FREE! Become a member on our website for more Premium Reso...
Video Transcript:
[Music] H what's up Ninja nerds in this video today we're going to be talking about ECG interpretation every clinician should have a very good systematic approach to how to read an ECG let's get into it one of the approaches that I think is pretty good from a lot of the textbooks and I think also maybe has some degree of clinical practice for myself is I like to first just determine what the rate is so I look at the ECG and I determine the rate the reason why that's important is it tells me if the patient's
Tac cardic or bra cardic right away or if they're just having a normal heart rate the second step is to determine what the rhythm is it narrow regular narrow irregular wide regular wide irregular it helps me to determine if they are tacac cardic what type of arhythmia are they having or if they are braidic cardic it also may give me an idea of what kind of like radiar rhythmia they're in step three as I'd like to look at the axis to determine if there's any deviation so left axis right Axis extreme right Axis deviation the
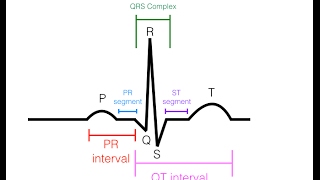
fourth thing is I like to evaluate the intervals I really like to look at the PR interval first because it helps me significantly in determining the different types of Brady rhythms especially AV blocks I also find it may give a little bit of benefit to finding wolf Parkinson's white syndrome and i' also like to look at the QT interval because the QT interval can help help me to determine the patient's risk of tors ODS to points I then like to assess the p-wave to see if there's any evidence of left atrial or right atrial enlargement
and then I like to look at the QRS complex to see if there's any evidence of bundle branch blocks like left bundle branch block right bundle branch block or ventricular hypertrophy right or left and then last I like to assess the ST segment and the t-wave to see if there's any evidence of myocardial lemia or infarction all right my friends now we're going to move on to the first step here which is we have to determine the patient's heart rate this is going to be the necessary thing right off the get-go so how do we
do this let's say that you see this ECG and it kind of seems stressful it's actually not that bad what I really want to do is I kind of want to zoom in on this Rhythm strip and show you guys how to calculate the heart rate so when we do that there's two different ways I prefer the r-wave method I find this to be very effective and basically what you do is you count the number of R waves that are present in the Rhythm strip in this particular scenario I count about 11 and then what
you're going to do is you're going to multiply those number of R Waves by six so it's 11 * 6 which is about 66 beats per minute that right there will give me the rate that the patient's heart rate is another way that you could do this is you could actually zoom in kind of on this particular area here and count the number of boxes that are present between so for example if we really looked at the nitty-gritty here I could actually average this out truly and I could say it's about 1 two 3 four
boxes there may be a little bit more here that it's extending outwards to but what you do is you take 300 and the reason why it's 300 is one box is indicative of like 300 beats per minute so what I do is I take 300 and I divide it by the number of boxes between one R wve and the other R wve it's about four boxes but it's just a little bit more to be very specific we're going to say it's about 4.5 boxes which comes out to about 67 beats per minute so that's the
two ways that you could go about determining the heart rate when you look at the ECG look at the Rhythm strip either count the number of R waves multiply by six or take the number of boxes between an r-wave and an r-wave and take that number of boxes and divide it from 300 and that should give you the heart rate once you've done that it's then pretty simple if the heart rate's greater than 100 beats per minute it's Tac cardia if it's 60 to 100 beats per minute it's a normal heart rate and if it's
less than 60 beats per minute it's there for bra cardia all right let's now move into the next portion here all right after we've determined the patient's heart rate we then want to determine okay let's say that the heart rate's too fast it's greater than 100 beats per minute in that scenario what I want to determine is okay their tacac cardic what kind of tartic Rhythm are they exhibiting so I like to then assess what's the actual QRS compx Lex is it narrow meaning is it less than 120 milliseconds three little boxes and is the
r to R interval regular what does that mean that means if I measured the distance from an r-wave to an r-wave it's the same all the way down the Rhythm strip there's a bunch of different types of narrow regular tacac cardias that I have to evaluate one is sinus tacac cardia the way that I evaluate this is that again heart rate's greater than 100 it's narrow QRS complexes as you can see here and the r to intervals are consistent what makes it different from the other three is that the p waves will be upright and
lead to inverted in AVR and every P wve will be followed by Qs complex for 2 to one atrial flutter there won't be any visible p waves instead and leads 23 avf they'll have these flutter waves which are very consistent also the heart rate tends to be very consist consistant at 150 and that's very very common for atrial flutter but again you'll notice a narrow QRS and you'll notice that the r to interval is the same and the last one is paroxysmal super ventricular tacac cardia this could be avrt like wolf Parkinson's white or AV
nrt AV noal re-entrant teoc cardia and what you're looking for is really no p waves and if sometimes you may be able to pick up like a retrograde p-wave but the big difference here is that there will not be any visible p-wave so that rules out sinus Tac of cardia and no flutter waves and this one can go pretty fast often times it can get up to 170s 180s you can get pretty fast with these guys and so that's the big difference often times we also use vagal Maneuvers and adenosine to really help to not
only diagnose this but also treat this type of disease what if I said I have a narrow irregular tack of cardia so heart rate greater than 100 beats per minute the QRS complex is narrow less than 120 milliseconds three little boxes and the artor interval is not the same every single time down the Rhythm strip I have three differentials atrial fibrillation would be one I got to look for these fibrillatory waves no obvious p waves are present that's a problem all right so if there's irregular and fibrillatory waves are present especially in lead one think
about atrial fibrillation atrial flutter with a variable block is also interesting because in this one you'll see that it's not constantly a 2 to one or it may be a 2: one a 3: one and it's bouncing back and forth where we have like two flutter waves three flutter waves and then a QRS complex so it's not the same so for example if I looked at this R to R this R to R and this one this one is completely different than this one this is again no fibrillatory waves I can definitely see that there's
some Sal tooth waves here but they're not consistent it's not always a 2: one it could be a 2:1 with a 3:1 and that's where you get the variability there and The Irregular of the artar interval the next one here is multifocal atrial tack cardio heart rate gred 100 bats per minute but here's the key difference I will see p waves but they'll all look different if I have three plus morphologically different p waves with a Tac cardia and irregular Rhythm and it's a narrow curus complex it's likely multifocal attac cardia again this is very
common in patients who have COPD I go to the next one I have a wide curus complex that's in this case is greater than 120 milliseconds or three little boxes all right that's common the r to interval if I calculate every R to R interval is always the same when you see this you think of intri attack of cardia until proven otherwise especially if all of this is the same this is monomorphic if I see whyde so again greater than 120 milliseconds are three little boxes of the Qs complexes and I see that the r
to interval is irregular so it's not the same every single time then I think about polymorphic ventricular Taco cardio with a prolong QT interval so you see how this patient they start having a prolong QT and then bang they go into torsades to points you can see how not every single one of these Q complexes look exactly the same morphology they're differing here it kind of gets a little bit bigger and then towards the center it kind of Narrows down and then gets bigger again and that's actually one of the classic looks is it gives
that kind of like ribbon look this is very consistent of polymorphic ventricular Tac cardio with a prolong QT also known as torsades to points and the last one is the most terrifying one this is usually ventricular fibrillation again you can see how all the Qs complexes are not the same morphology they're not always exactly the same type of morphology the same distance so therefore again this is wide and it's not the same R to interval therefore it is irregular this is ventricular fibrillation you see this you get kind of scared right but that's important to
be able to identify so tacac cardia you want to know is it narrow wide regular irregular and that'll generate your differentials now with that being said let's go to a patient who has a braed cartic rhythm so they heart rate's less than 60 beats per minute then I got to start thinking okay could they have sinus braic cardia or could they have an AV block all right well the first thing I want to do is look at the PR interval if the PR interval is normal they don't drop any QRS complexes and every p is
followed by a QRS and it's again well that's sinus bradicardia if my PR interval is prolonged every p wve is followed by a Qs complex but I don't drop any qrs's you know how it's out every p-wave QRS p-wave QRS p-wave QRS nothing changes there's no droppage of the QRS but they're the PR interval is prolonged in comparison to this one in that particular scenario if it's greater than 200 milliseconds the per interval this patient has a first-degree AV block go to the next thing the pral seems to be getting longer every single time so
it gets longer longer longer and then here's the P wve but then look what happens here I don't have a QRS complex I dropped my QRS complex so here I had a pro I had a prolonged but this one is prolonged and it's getting progressively longer and then I drop a QRS these are not the same this is a second degree AV block moit one it's longer longer drop you have a winky Bo what else if I have have a PR interval that is prolonged but it's constant it's not changing it's not like 160 it's
not let's say 200 220 240 260 it's not getting progressively longer it's constant and then what you notice is pqrs pqrs p no QRS I drop a QRS with a constant PR interval this right here my friends is a second degree move it's two and the last one is that there's literally no relationship there's just a ton of p waves and then there's no QRS that are constantly correlating with that if you see a ton of p waves with no correlating QRS and on top of that the p waves are beating at their own rate
that's super suggestive of again a AV disassociation so if the Atri are beating at their own rate the ventricles are beating at their own rate and it's even wide complex that suggests an infranodal AV block this is super consistent with AV disassociation which is very indicative of a third degree a block so again look at the rate determine if they're bra cardic tacac cardic then take that to the next step is it a narrow regular tacac cardia narrow irregular wide regular wide irregular then it's braad cardic do they have sinus Brady what's their PR interval
is it prolonged is it a first degree is it prolonged and dropped is it a second degree M it's one is it constant and then dropped second degree M it's two is there no relationship between the PES and the QRS complexes it's a third degree I just determine my rhythms Isn't that cool the next thing is we said axis so I I looked at my rhythm right I looked I looked at my rate I looked at my rhythm now I'm going to look at the axis okay cool how do I look at axis all right
well the first thing I got to do here is I'm going to look at lead one and what I want to look at is I want to look at the QRS complex is I want to see with the deflection where is the most positive deflection is it upwards or is it downwards in this one it's upwards so what I want you to do is I want you to take your left hand and lift up your thumb all right so that's going to be thumbs up on that side all right that's the first thing I do
second thing I do is I have to look look at avf what's the QRS complex looking like is it upwards deflection or is it a downwards deflection this case it's upwards get that thumb up when both thumbs are up it's normal baby that's a normal axis there's no true underlying pathology here now in left axis deviation is different look at lead one what's the QRS it's predominantly positive all right cool thumbs up with the left hand then look at avf o the Qs comp this is predominantly negative so the right thumb is going to go
downwards so if I have that you would think okay this is left axis deviation because the thumb that's always pointing up is usually indicative of which axis is deviated but you got to be careful so in this particular scenario what I would do is when I see upright and negative just be very careful because this still could be a normal axis look at lead two and if you look at lead two and and you see that it's predominantly negative here that definitely confirms that it's actually going to be what left axis deviation but if you
looked here and it was predominantly positive then it would be a normal axis but again I look here up I look here down I look here and it's predominantly appears negative and or you could even say equipas that is indicative of left axis deviation question is is what causes left axis deviation it's usually anything that alters the depolarization of like the left ventrical all right usually via like the bundle system so I think a good couple examples here would be a left bundle branch block that's a very common one left ventricular hypertrophy which can actually
cause a lot of strain and stretching of the left bundle branch and on top of that a left anterior facular block can also cause a left axis deviation all right what about right Axis Dev deviation okay look at lead one it's predominantly negative thumb down go to lead avf predominantly positive so I got this one down this one up that's right Axis deviation baby the thumb that's pointing up tells me what the actual kind of deviation it is so then I got to think about it there's something wrong with the right ventricle it's either a
right bundle branch block right ventricular hypertrophy or left posterior facular block so left axis is left bundle left ventricular hyper left anterior facular block right Axis right bundle right ventricular hypertrophy left posterior facular block the last one is Extreme right Axis deviation I think if you saw this you wouldn't be worried about axis you'd be worried about does this Pati have a pulse or not but the concept Remains the Same if you're evaluating axis what's the lead one show it shows a downward deflection predominantly so the thumbs down with the left if you look at
avf what does it show is there's a predominant downward deflection and in this case here if both thumbs are pointing down that's extreme right Axis deviation the most common ethology of this is usually monomorphic vac all right so we've then said okay what's the rate is it a tartic rhythm a bra aaric Rhythm which type is it then we also evaluated the axis is it normal is it left axis if it is could it be due to left B branch block left incopy left inter cular block is it a right Axis deviation in that particular
scenario again could it be right bundle branch block right ventricular pervy left posterior fix cular block or is it extreme right Axis which you can see in vtac you can also see invariance of wolf Parkinson's white syndrome we go to the next thing approach to intervals there's two intervals I think are very important to remember one is the PR interval and the other one is the QT interval the question I want you to know is is the PR interval prolonged or shortened now if it's prolonged that tells me about AV blocks right for example if
it's greater than 200 milliseconds right that's prolonged in this case it could be a first degree EV block if I don't drop a QRS it could be a second degree moitz one if I drop a QRS as it gets longer and longer and longer if it's a constantly prolong PR interval and I drop a QRS that could be indicative of a mobit 2 and third degree AV blocks you're going to see these super abnormal multiple frequent p waves with no true relationship between the actual patient having a atrial and ventricular Association all right that's pretty
straightforward right for sure this one's not as high yield but it is important to think about this because one disease that actually may come up in your exams is Wolf Parkinson's white syndrome this one can have a very short Peri interval less than you know 160 milliseconds the concept behind this is look for two other findings so there's a Triad there is a Delta wave which is this kind of brief upstroke here there is the very very kind of like short PR interval here and then there's that kind of wide Qs complex that's usually indicative
of wolf Parkinson White syndrome via the bundle of Kent then I like to look at the QT interval so I like to measure between this part here coming all the way to the end of the t-wave and knowing what that QT interval is now it is important to remember that this can vary based upon male female and there's a lot of different numbers I like to remember basically if the pro if the QT interval is greater than half of the r to R interval so the distance between this r-wave and this R wve if that
QT is greater than half that is prolong sometimes I like to just remember also if it's greater than 500 milliseconds in that particular situation these patients are super high risk for something called torsades to points the causes you have to be thinking about here include drugs such as anti- rhythmics like amiodarone abuti antibiotics such as macrolides anticho like halap paradol quene anti-depressants such as ssris and tcas anti tics like andron or Compazine and here's the big ones baby hypokalemia hypomagnesemia and hypocalcemia these can all prolong the QT increasing the risk of T torsades to points
that's important to remember the Short QT interval I wouldn't worry is much about too significantly but do remember that if the QT interval is very very short like less than maybe like 460 potentially um it does create the slight increase risk for tacac cardia so you may see this with Hyper calcemia and Hyper calmia not as high yield though all right that's intervals we now go to the p waves to determine if there's atrial enlargement so when I look at the p waves I want to know does the patient have left atrial enlargement or right
atrial enlargement so I'd like to look at lead 2 first when I look at lead 2 and I really zoom in here here I kind of see this configuration when I zoom in you see how the p-wave appears to have like a split we call that a biit p-wave when you see bit p waves and lead two that makes me think about left atrial enlargement so then what I got to do is I got to confirm that and I go to lead V1 and when I look at V1 I want to see a basic p-wave
and if I see the basic P wve but I see here that the terminal component is bigger than this little initial component if I fill that in there that's definitely indicative of left atrial enlargement and that's super important because there's different reasons why patients could have left atrial enlargement their left atrial pressures could be high because their left ventricular pressures are high in the scenarios of left heart failure it could be due to a cardiomyopathy that creates elevated left ventricular pressures or it could be due to mitro valve diseases that cause left atrial pressures to
be high in the scenario like mitro valve stenosis example is that would be all right what if I saw this one where I look here and I say oh shoot that P way be big Baby that thing is greater than greater than or equal to 2.5 millimeters in this particular scenario that's a very high peak type of p-wave if I see that I'm thinking radiat enlargement but I got to confirm so I'm going to go to V1 and when I go to V1 I should see a basic p-wave but the comparison between left and right
atrial enlargement the initial component should be larger than the terminal component and if I see both of these it's highly indicative of right atrial enlargement and I want to think about what usually pulmonary hypertension can create elevated right ventricular pressures and as a result cause right atrial enlargement or truspa disease such as trios stenosis all right that's not too bad right all right we get to the QRS complex now I want to know does the patient have bundle branch blocks or ventricular hypertrophy all right so let's say I want to assess these patients for bundle
branch blocks potentially well how do I do that I like to look at V1 and V2 first all right and what I want to see is I want to see something called an RS wave I just want you to really look here for a very deep s-wave in V1 and V2 so you see how there's like this little r-wave and then boom you see this huge huge s-wave here right when I see a very large s-wave in the V1 and V2 precordial leads and then I see this very large notched like r-wave in V5 or
V6 this is super super suggestive of a type of bundle branch block and usually this is indicative of a left bundle branch block now left bundle branch blocks what's important to remember with this one one is it's usually due to something that's like stretching or thickening the left ventricle so this could be due to left heart failure right especially systolic heart failure it could be due to myocardial infarction which kind of kind of knocks off the left bundle branch block or the left bundle branch you could actually infar it and cause fibrosis of that bundle
branch or left ventricular pery where you thicken that actual myocardium and compress on the left bundle branch this is very common when I see this next concept I see this r s r Prime wave and V1 V2 or I see the M that automatically makes me think about a right bundle branch block what would even confirm it more is if I looked over at V5 and V6 and saw something interesting here if I see like this wide slur like swaave so you see how it goes q r and then look at the swave you see
the distance here right here that wide slurred type of s-wave that is so so suggestive there of a what a right bundle branch block so the combination of these two right bundle branch block baby what would cause that something that's going to stretch out the right ventricle or thicken the right ventricle or infar parts of the right bundle branch block pulmonary hypertension will cause right ventricular hypertrophy maybe even right ventricular dilation and myocardial infarction like a right ventricular Mi could also kind of cause fibrosis of the right bundle branch all right so that's blocks what
about hypertrophy now well with hypertrophy I want to look again at V1 and V2 and I want to see what these S waves do so if these s-waves are like crazy deep I'm talking insanely deep here right and then I go ahead and I look over at V5 and V6 and I see that these R waves are like through the roof that's super suggestive of left ventricular hypertrophy now there is different criteria that you can do so you can add up the amount of boxes of the swave and then add up the amount of boxes
of the r-wave and if it's greater than 35 mm it's usually suggestive of left ventricular hypertrophy and that's one thing that we could do but if I see a super deep swave and a very large r-wave I definitely want to be thinking about left ventricular hypertrophy right this is super common in patients who have like aortic stenosis or hypertension now with right ventricular hypertrophy I want to see very tall R waves in V1 and V2 very tall R waves and then I want to look over in V6 and what I want to see is I
want to see the S waves being much bigger than usual they're definitely not usually this big and so when I see this that definitely gives me the idea of what's called right ventricular hypertrophy so then I would be thinking again about pulmonary hypertension is a very very common cause here all right all right we move on to the next component here and this is the Behemoth this is where it really counts you can't miss some of this stuff here so I want to talk about how do we approach the ST segment in the t- waves
especially if a patient comes in with angena so chest pain when you assess the St segments you want to know does it look like it's depressed so in other words when I look at the J point where does it look in comparison to this kind of iso electric line if that is depressed greater than 0 .5 mm in V2 and V3 are at least greater than 1 millimeter in all other leads and it has to usually be contiguous that's consistent with SD depression the other thing I like to know about SD depression is morphology I
want to know does it look like it's horizontal because that's concerning for aeia does it look like it's down sloping that's also concerning for aeia the one that's maybe not as concerning could be UPS sloping but if I see horizontal and downs sloping St depressions and it meets this criteria greater than 1 millimeter depression again from you have an ISO El electric line here and the J points at least greater than a millimeter below that all right or greater than 0.5 millim in V2 and V3 and you see horizontal down sloping type of configuration and
it needs to be two contiguous leads this is concerning for esema myocardial esea such as an unstable angena or n stemi if I see t-wave inversions here so you see how this t-wave usually it's supposed to go whoop and it's inverting here that's definitely concerning for esea right and so if I see a combination of these two particular findings I definitely want to start asking myself the question what's the troponin level if the troponin level is normal that tells me it's unstable Ana right because there's no myocardial infarction if the tronent is positive it tells
me that there is myocardial inunction it's prob subendocardial and this is an end stemming and that's super important to be able to pick up my friends we call this non-st segment elevation acute coronary syndrome because acute coronary syndrome is consisting of an stemi stemi and unstable Anga so if you see ST depression t-wave inversions and this STD depression is horizontal or down sloping be concerned check the tronin and determine if it's unstable Anga or in stemi now not everything estd depression and t-wave inversion is always acute coronary syndrome I think it's also you know Wise
to consider alternative diagnoses like dioxin toxicity so you could check a dexin level or hypokalemia so you could check a potassium level all right with st elevation if I see St elevation what does that mean that means when I look at the J point it's usually greater so if I have an isoelectric line here and I look at this portion right here how much higher is it above this isoelectric line if it's greater than 1 mm right and the Lim leads what does that mean it means you know two three avf one AVL AVR if
it's greater than 1 millim any of those leads and it has to be two contiguous ones for example two and three like lead two and three you would have to have SD elevation in both of those not just one of them or greater than two millimeters in the precord Le what does that mean it means you have to have greater than 2 millimeters two of these actual box two little boxes here right has to be above the isoelectric line by two little boxes or one little box if it's elevated above that that actual isoelectric line
the J point or the ST segment and it's in V1 V2 V3 V4 V5 V6 at least two of those contiguous leads can't just be one that's concerning all right that's very very concerning for myocardial lemia but here's what I really want you to also consider here which is the morphology of the ST segment elevation now this isn't always perfect but if it has a smiley face appearance concave that's less suggestive of myocardial esmia it could be more indicative of like benign early repolarization or pericarditis maybe even hyperkalemia right here's another type of concave configuration
just another type of look of it if you see convex though that's a that's a not a smiley face that's a frowny face that's more indicative of infarction myocardial infarction and it's way more concerning of a configuration here's just another way look like that call the tombstone effect this is very concerning for myocardial infarction so not just elevation cons contiguous leads but also configuration helps me to identify if there is a concern of stemi right that is really going to be present here and then don't forget to check your tronent because if I have an
st elevation and tronent elevation it may make me think about a stemi now hyperacute t-waves believe it or not can actually sometimes be be a find ing of es keemia that can prede EST elevation so sometimes patients will come in with Hyper QT waves that then start to bump into EST segment elevation so just remember that maybe they don't come in with st elevation but they come in with this large broad type of t-wave here this may precede them going into this tombstoning ST segment elevation so this could be an early indicator of myocardial infarction
that then will then progress to this all right so either way when I see STL elevation or hyper QT waves my first thought is a stemi so then I have to start thinking about where's the St elevation where's these hyper QT waves I got to localize the stemi right so how do I do that well the first thing it's important to do is remember your leads so when I look at the ECG I have to kind of have St elevation and particular leads to determine what type of stemi it is for example if it's an
anterior stemi you have like anterior seal so V1 V2 V3 V4 so if I see St elevation here and V2 V3 and V4 and on top of that you know what else suggest stemies more than things like pericarditis binly repo hyperemia is reciprocal changes and especially these reciprocal changes can occur in like 2 three avf so if I have reciprocal changes Plus St elevation in like V2 V3 V4 this is super suggestive of an anterior Mi if I look here two I see St elevation three St elevation avf St elevation and reciprocal changes in one
and AVL and look at the configuration of this thing this Con convex right this is an inferior Mi that's an inferior Mi the next one is lateral that's usually one AVL V5 V6 so St elevation here in one St elevation here in AVL St elevation of V5 and St elevation V6 and again all it's got to be is it's just got to be in these particular two 2 mm and over here 1 millim and if I have that in two contiguous leads which I do in this one look I got a one I got an
A I got a B5 V6 this is a lateral usually what we refer to as a high lateral stemi and you see reciprocal changes in two three and avf what does reciprocal changes means that means that you'll see STD depression or like t-wave inversions the last one's a posterior stimy so oftentimes what I like to do is I like to look at V1 V2 and V3 and I look for t-wave inversions and St depressions so You' then say oh maybe this patient has like an inst stemi it's important to always have a high degree of
Suspicion for a posterior M so what you do is you take the leads and you put them on the posterior chest wall and so you do something where you actually change it to V7 V8 v9 and you'll see here that they have St elevation and V7 V8 v9 so they have ST depression t-wave inversions in V1 V2 V3 slap on the posterior chest leads V7 V8 v9 it's SD elevation that's a posterior stemi so you see now why it's super important to see oh SD elevation it's there all right based upon the actual numbers of
elevation above the isoelectric line you see the STD segment but then notice where it is if there is that presence of the St elevation what's the morphology it convex concave it can provide some you know some justification if it's truly more concerning for ES schia then look at where it is is it in the anterior V1 to V4 and does it have reciprocal St depressions and t-wave inversions that could be an Anor stemi is it in 1 AVL V5 V6 reciprocal uh you know changes seen that could be you know some type of lateral stemi
is it in 23 avf reciprocal changes are seen that could be an inferior and if you see SD depression t-wave inversions with V7 v9 they posterior leads St elevation there could be a posterior semi and all of these scenarios you should rule those out first and once you've done that then you consider things like pericarditis pericarditis often times will also be associated with diffuse St elevation you'll see it in almost all the dang leads on the EKG but then also have what's called PR segment depression also the morphology is usually a concave morphology and then
hyperkalemia I have seen this also cause ST segment elevation uh usually it'll come with those Peak te- waves or hyperacute te- waves again it's important for this one it's really difficult to diagnose sometimes you have to just check a potassium for these patients all right my friends that covers ECG interpretation I hope it made sense I hope that you guys enjoyed I hope you now have a good approach and you're able to T tackle any ECG that comes your way all right Engineers love you thank you and as always until next [Music] time [Music]
Related Videos

1:01:14
Arrhythmias | Clinical Medicine
Ninja Nerd
180,872 views

1:19:14
EKG Basics | How to Read & Interpret EKGs:...
Ninja Nerd
2,671,129 views

1:00:01
It's time to fall asleep and relax your bo...
Kagura Rain
8 views

52:22
Coronary Artery Disease | Clinical Medicine
Ninja Nerd
186,998 views

59:14
MASTER ECG/EKG INTERPRETATION: A Systemati...
Ninja Nerd
1,932,277 views

37:58
Atrial Fibrillation | Clinical Medicine
Ninja Nerd
68,029 views

58:20
Congestive Heart Failure | Clinical Medicine
Ninja Nerd
286,343 views

20:44
How to Read an ECG | ECG Interpretation | ...
Geeky Medics
328,620 views

48:44
EKG Rhythms | ECG Heart Rhythms Explained ...
RegisteredNurseRN
855,624 views
12:24
EKG/ECG Interpretation (Basic) : Easy and ...
MINT Nursing
6,249,079 views
12:14
Most Common ECG Patterns You Should Know
Rhesus Medicine
1,627,133 views
41:56
Hypertension | Clinical Medicine
Ninja Nerd
220,233 views

26:57
ECG Interpretation Made Easy; How to read ...
MedNerd - Dr. Waqas Fazal
659,174 views
46:42
Valvular Heart Diseases | Clinical Medicine
Ninja Nerd
163,085 views

29:44
From Basics of 12 Lead ECG to How Waves ar...
Nonstop Neuron
255,827 views

3:00:35
EKG Interpretation | Master Fundamentals o...
Dr. Najeeb Lectures
6,502,303 views
38:13
Pericardial Diseases | Clinical Medicine
Ninja Nerd
56,310 views

18:31
Understanding Arrhythmias
Zero To Finals
102,534 views

16:33
Rapid, structured ECG interpretation: A vi...
The Learn Medicine Show
98,240 views

15:04
Myocardial Infarction / STEMI on ECG - Pra...
MedCram - Medical Lectures Explained CLEARLY
320,308 views