Pleural Effusion (DETAILED) - (pathophysiology, signs and symptoms, treatment)
358.63k views2167 WordsCopy TextShare
Armando Hasudungan
Where do I get my information from: http://armandoh.org/resource
Facebook:
https://www.facebook.com...
Video Transcript:
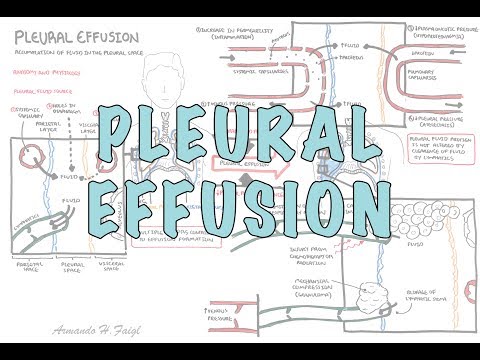
hello in this video we're going to talk about pleural effusions pleural effusions is where you have accumulation of fluid in the pleural space let's recap some basic anatomy and physiology so here are the lungs surrounding the lungs is the visceral pleura which continues on and becomes the parietal pleura which attaches to the thoracic wall the visceral and parietal pleura is a continuous serous sheet the space that separates them is the pleural space which contains pleural fluid let's take a closer look here is the parietal pleura layer and attached to the lung is the visceral pleura
layer in between is the pleural space where we find pleural fluid the visceral space is really the lungs which contains the pulmonary capillaries and the alveoli the parietal space is a thoracic wall where we find the systemic capillaries in the parietal space you also find lymph vessels which drain the pleural fluid from the pleural space the pleural fluid comes from three main sources the main source being the systemic capillaries then you also have fluid that can enter from the pulmonary capillaries and also from the abdomen where fluid can come in through small tiny holes in
the diaphragm again the lymphatics drain this pleural fluid and helps maintain the normal pressure in the pleural space so pleural effusions is essentially where you have a cumulation of pleural fluid in the pleural space when this happens you really get restriction of lung expansion and so you get shortness of breath there's two main mechanisms for developing fertile fusions the first is we have too much pleural fluid forming in the pleural space and the second mechanism is where you have decrease in pleural fluid clearance from the pleural space let's take a look at some examples of
the first mechanism where you have an increase in pleural fluid formation let's zoom into the right lung here where we find a pleural effusion here again you can have your pulmonary capillaries part of the your visceral space and here are your systemic capillaries which are part of your parietal space imagine in either the pulmonary or systemic capillaries you have inflammation this will trigger the vessel cells to contract causing an increase in vascular permeability when there is an increase in vascular permeability fluid and proteins will leak from the vessels into the pleural space which increases fluid
formation essentially in the pleural space and so leads to pleural effusions the capillaries leaving the plural membrane will return to the hot eventually via the veins if there is an increase in venous pressure such as left-sided or right-sided heart failure this can lead to pleural effusion because blood cannot travel back to the heart efficiently another cause of pleural fluid formation can be if there is a decrease in plasma oncotic pressure which for example means when you have low amounts of protein in the blood because there's no proteins or not enough proteins in plasma this means
fluid cannot be kept within the vessels and so it will leak out into the interstitial space another cause of increase in pleural fluid formation is if you have a decrease in pleural pressure such as in lung collapse or atelectasis these are some examples of things that can cause an increase in pleural fluid formation note that in some of these examples proteins also move into the pleural space causing an increase in protein levels in the pleural fluid pleural fluid protein levels are not altered by clearance of fluid by the lymphatics this is very important as protein
levels in plural fluid helps differentiate between two types of pleural effusions anyway we'll talk about this later the second mechanism of developing pleural effusion is when there is a decrease in pleural fluid clearance which we sort of touched on the lymphatics let's now take a look at some examples that cause a decrease in pleural fluid clearance remember fluid is cleared from the pleural space by the lymphatic system if you have a blockage of the lymphatic stoma this means less fluid drains leading to pleural effusion if there is an obstruction compression obstructing the lymphatic drainage this
means fluid cannot be trained an example is if you have a granuloma in the lung for example compressing against the lymphatics another example is if there is a increase in venous pressure because if you think about it the lymph vessels eventually will drain into the venous system so if there is a buildup of pressure in the veins this means buildup of pressure in the lymphatics and so the de lymphatic system cannot drain adequately cancer invasion can block and disrupt fluid drainage leading to pleural effusions chemotherapy and radiation can also damage the lymph vessels finally if
there is limitation of respiratory motions this decreases the draining rate because as we know the lymphatics and vessels also rely on contraction of muscles to support the movement again the two main mechanisms of chloral fusion are increase in fluid formation and decrease in fluid clearance and we learned a few examples of each however it's very important to know that pleural effusions don't occur from a single factor we talked about usually multiple factors contribute to pleural effusions pleural effusions usually present with an underlying disease such as pneumonia the clinical findings of pleural effusions specifically includes shortness
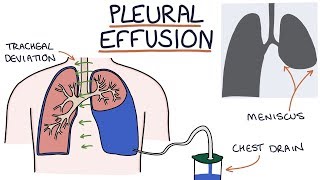
of breath because the fluid prevents proper ventilation and lung expansion if you percuss the lung basis they will be dull there will be also decrease chests war movement on the affected side because the fluid restricts the movement here on auscultation there will be decreased breath sounds around where the fluid is investigations to order include a chest x-ray and on the x-ray you will find blunting of the costophrenic and cardio phrenic angles which signifies a fusion here is a chest x-ray of someone sitting down you can see straight away that there is a large pleural fusion
on the left hand side there's blunting of the coast oh and cardio phrenic angles and there's also the meniscus sign the darker pink on the top here again is another chest x-ray and again you can see the classic meniscal sign here's a less subtle one a bilateral pleural effusion you can see blunting of the costume and cardio phrenic angles bilaterally and also the meniscus sign just if someone prevents with suspected pleural effusion of unknown cause initially blood tests such as full blood count EUC and lfts can be helpful the diagnosis of pleural effusion gold standard
would be an ultrasound and looking for the specific cause of the pleural effusion thora Kherson tsys is warranted thoracentesis is where they stick a needle in between the ribs with guidance of the ultrasound and then fluid is drawn up for fluid analysis thoracentesis is both diagnostic and therapeutic thoracentesis gets you a pleural fluid sample which can be then analyzed initially you would order lactate dehydrogenase and protein levels here this will help differentiate the two main types of pleural effusions of the two categories of pleural effusions which are translated pleural effusion and exudative pleural effusions this
is where we bring in what's called Lyte's criteria and latts criteria will essentially tell you if the pleural effusion is from an exudate ofcause or translate ofcourse exudative requires one of the following where you have pleural fluid protein to serum protein ratio greater than 0.5 which really means that it will be exudate if there is more protein in the pleural fluid the second is where you have a pleural fluid lactate dehydrogenase to serum lactate dehydrogenase ratio greater than 0.6 which really means it's exudate if the plural LDH level is higher or finally it is an
exudative plural fusion if the pleural fluid LDH is greater than two-thirds the upper limit of the laboratory normal value of serum LDH unfortunately the lights criteria miss identifies 25% of tragedy to diffusions as exudative infusions now if transit ativ effusions is suspected based on clinical presentation or laboratory findings other things can be analyzed within the pleural fluid such as your brain naturally peptide which if very elevated signifies heart failure causes of transitive pleural effusion include congestive heart failure with elevated brain naturally peptide liver cirrhosis and nephrotic syndrome and also superior vena cava obstruction exudative pleural
effusions really means that there is a lot of LDH and/or a lot of proteins in the pleural fluid in comparison to the serum levels if exudative pleural effusion is suspected and you want to diagnose a potential cause of exudative pleural effusions other tests you can order here include pleural fluid microscopy culture sensitivity pleural fluid cell differentiation and pleural fluid glucose levels these tests can help identify potential causes of the exudative pleural effusions some of the more common causes of exudative pleural effusions include infections malignancy pulmonary embolism gastrointestinal pathologies such as pancreatitis and connective tissue diseases
now the management of pleural effusions briefly obviously you can treat the underlying cause thoracentesis is helpful to identify the potential cause but also can be therapeutic if the fusion is large enough the definitive treatment is a chest train where a tube is inserted into the pleural space to drain the fluid out you can see on this x-ray on the left hand side you have a pleural effusion and a tube inserted in the safe triangle which will drain the fluid out floral desus can also be used if pleural fluid continues to build up within the pleural
space despite the chest during being used pleurodesis is used in conditions such as cancer where fluid is continuously formed pleurodesis is a procedure where dr. cyclin or talcum powder are put in within the pleural space to obliterate the pleural space to prevent recurrent pleural effusions or even pneumothorax Fleur ectomy is a surgical option which removes the pleura all together let's now look at some different causes of pleural effusions specifically in more detail beginning with transudative pleural effusions first looking at heart failure so normally the pulmonary artery's pumps blood to the lungs where I'll return to
the left side of the heart imagine you have left ventricular failure main cause of heart failure this causes fluid to go backwards to the pulmonary vein pulmonary capillaries when fluid goes backwards it will result in pleural effusions bilaterally let's take a closer look at how this happens here are the pulmonary capillaries the pulmonary interstitial and the pleural space if there is left ventricular failure pressure builds up here and blood can pull in the pulmonary capillaries this results in fluid moving into the pulmonary interstitial initially causing pulmonary edema then fluid can shift to the pleural space
closing pleural effusions usually the lymphatics can help maintain equilibrium but with so much pleural fluid being produced there is less lymphatic drainage causing pleural effusions again here the pleural fluid typically has raised brain naturally peptides B and P which is a marker for ventricular strain other causes of translated pleural effusions we talked about was liver cirrhosis and nephrotic syndrome there are many factors which lead to pleural fluid in these examples but the main one would be low protein levels in the blood in liver cirrhosis there is a decreased protein production such as albumin the main
protein that circulates in our blood in the photic syndrome there is an increase in protein loss there is increase in albumin lost through urine both liver cirrhosis and nephrotic syndrome means that there is low protein levels in the blood hypo protein emia or hypo alder anemia this means that there will be a decrease in oncotic pressure in the vessels due to their low protein levels which means that the vessels can't hold the water within the vessels and so water will shift into the pleural space as a result causing the pleural effusions exudative pleural effusions are
the pleural effusions with high LDH ad or high protein levels in the pleural fluid compared to serum examples include malignancy malignancy can cause effusions in many ways it can obstruct the storm of the lymph vessels it can compress the lymph vessels itself 75% of malignant infusions are from lung breast and ovarian cancer finally pulmonary embolism is a cause of pleural effusions exudative pleural effusions and probably an unrecognized one hominy embolism or PE occurs when there is a thrombus which occludes a pulmonary artery or pulmonary capillary here as shown when this happens the pulmonary vessels will
compensate in a few ways one way is that it will cause shunting of blood flow to capillaries which work which means more blood flow which means more fluid can enter the pleural space there will be an increase in vascular permeability there and fluid will start to shift into the pleural space I hope you enjoyed this video on polar fusions thank you for watching you
Related Videos
9:38
Superior vena cava and the azygos system c...
Armando Hasudungan
146,781 views

53:42
Pleural Diseases: Pleural Effusion, Pneumo...
Ninja Nerd
56,026 views

9:09
Pleural Effusion - causes, symptoms, diagn...
Osmosis from Elsevier
1,114,000 views

10:30
Asthma - signs and symptoms, pathophysiology
Armando Hasudungan
1,008,544 views

23:38
Pleural Effusion - Transudate or Exudate -...
Medicosis Perfectionalis
140,510 views
11:40
Interstitial Lung Disease (ILD) - Classifi...
Armando Hasudungan
189,966 views
6:37
Understanding Pleural Effusions
Zero To Finals
491,349 views

25:09
Introduction to respiratory system anatomy
Sam Webster
45,969 views
31:41
Respiratory | Mechanics of Breathing: Pres...
Ninja Nerd
1,860,806 views
12:36
Cardiac Tamponade - pericardial effusion, ...
Armando Hasudungan
107,038 views

12:38
What is a Pleural Effusion? EXPLAINED!
ICU Advantage
64,306 views

46:22
Chronic Obstructive Pulmonary Disease (COP...
Ninja Nerd
141,460 views

17:34
Understanding COPD - causes, signs, sympto...
Talking With Docs
44,065 views
29:34
Respiratory Failure | Clinical Medicine
Ninja Nerd
53,423 views
38:06
Acute Respiratory Distress Syndrome (ARDS)...
Ninja Nerd
64,957 views
8:02
Pleural Effusions - Causes, Diagnosis, Sym...
MedCram - Medical Lectures Explained CLEARLY
217,046 views

25:11
ARDS (Acute Respiratory Distress Syndrome)...
RegisteredNurseRN
1,491,909 views
27:14
PLEURAL EFFUSION | Causes | Approach | Dia...
Medi - Lectures
41,884 views
30:23
Chest Tubes
Ninja Nerd Nursing
20,099 views
9:18
Pleural Effusion Explained Clearly - Cause...
MedCram - Medical Lectures Explained CLEARLY
322,284 views