Cardiovascular | Structures and Layers of the Heart
1.17M views4098 WordsCopy TextShare

Ninja Nerd
Official Ninja Nerd Website: https://ninjanerd.org/
Ninja Nerds,
In this lecture Professor Zach Mur...
Video Transcript:
all right Ninja nerds in this video we're going to talk about the anatomy of the heart as well as the layers of the heart so first off a little bit about the anatomy of the heart where would you actually find it well you'd find it within the thoracic cavity but you'd find it within a special cavity in the thoracic cavity called the mediastinum so it's actually found within What's called the media stum there's actually different components and of the media stum like this Superior medyum the central anterior and posterior medyum we're not going to get
into all that another thing about the heart is not only is it situated within the medus stum but it's actually shifted about 2/3 to the left of the midsternal line okay so it's kind of shifted to the 2/3 to the left of the midsternal line that's another important thing so when you look at the apex of the heart is actually pointing towards your left hip and the base is actually pointing towards your right shoulder another thing about the heart is that it's actually going to weigh approximately about 200 to 300 G they generally say it's
about the size of a fist okay so that's kind of the just basic concepts about the heart and again Apex is pointing towards the left hip and then the actual uh base is pointing towards the right shoulder now when we look at the heart we actually see a bunch of different chambers with inside of the heart for example if you look here you see these two top Chambers here these two top Chambers are called your Atria right so plural form is the Atria but for example since this is going to be on the right side
of the heart this is on the left side of the heart this is referred to as the right atrium and this one over here is referred to as the left atrium the big difference between these is what is actually going to be filling them also so for example if you look at the right atrium it has three big vessels that are emptying blood into this cavity one is this bad boy right here this structure right here is actually called called the inferior vena it's a big vein that's bringing blood from beneath the diaphragm from the
lower appendages right as well as some of the abdominal viscera and a lot of different other structures so this structure is called the IVC which is called the inferior vnea then you have the one that's above the diaphragm bringing blood from the head the neck and even the upper limbs so this is going to be called the superior vena so we have the inferior vena superior vena and we have another vessel that's emptying blood in here what is this structure here called this structure is actually emptying blood into the right atrium too and this is
called the coronary sinus so it's the opening of the coronary sinus which is one of the structures that is basically taking blood from The myocardium the heart and returning it back to the right atrium you also have a little bit of scar tissue in this area you know whenever uh you're born generally there's a hole between the right atrium and the left atrium called the fal Val but whenever the actual fetus starts growing up and stuff like that the actual hole basically closes up and becomes a lot of scar tissue so imagine here I kind
of draw like a little bit of scar tissue here and this Scar Tissue right here is representing What's called the fossa ovalis which used to be the fan oval in the fetus okay so they call this one here the fossa ovalis okay so that's that another kind of important thing about this is that there's some specialized not cells we talked about this in other video so we're not going to spend a lot of time here but there's another like nodal cell a bunch of different types of nodal cells which are Auto auto rhythmic cells they
can generate Action potentials and set your sinus rhythm it's called your SA node and we even talked about it more we had one right here which would be the AV node then we'll go into the bundle of hiss the right and left bundle branches and the penji system we're not going to talk about all of that right now okay we do that in another video on the intrinsic cardiac conduction system all right so that covers that part now there's the next thing the left atrium what's emptying blood into the left atrium the left atrium is
receiving blood from a couple different structures here it's all the same but they're basically bringing blood these structures here and over here it looks like it's emptying blood into this side of the heart but it's not it's coming around from behind the heart and it's dumping in over here so imagine it's dumping in over here from these two little red veins over there these guys are emptying blood into the heart and what's really important about this is that these veins are emptying blood that are coming from the lungs from the pulmonary circulation so because of
that these are called pulmonary veins so these guys right here are called your pulmonary veins and they're really important because they're bringing oxygenated blood from for example we said that this is the left side of the heart this is the left pulmonary veins bringing blood from the left lung whereas over here what do you think these are called These are the right pulmonary veins and the right pulmonary veins are bringing blood from the right lungs but remember both the right and the left pulmonary veins are emptying blood into the left atrium Okay now what's that
what else is really important about this we covered that well now we got to talk about what is this partition here in between the Atria and the ventricles these are called Valves and they basically are pro providing a one-way flow we don't want things to come back right so what happens is what is this valve right here called this valve right here is a special valve this is called the tricuspid valve so you can call it the tricuspid valve or another name for it as you can call it the right atrio ventricular valve because it's
separating the Atria from the ventricles so that's why you can call it atrio ventricular valve and it's on the right side this one over here which is separating the left atrium from the left ventricle is called the bicuspid valve the bicuspid valve or another name is the the mital valve or the left atrio ventricular valve because it's separating the Atria and The ventricle on the left side now a little bit of thing about this valve here is if you look at it it's actually kind of cool because it's layered really really nicely when you look
at the inner part of it it's actually consisting of different layers so it actually has a couple layers in here and it has a lot of collagen and elastic tissue on both sides and it also has a little bit of uh other different types of spongy tissue in here it's actually made up of two different layers called the Zona spongiosa the Zona fibrosa and even another one called the Zona petric and there's uh endothelia lining around it so just so that you know the valve is actually made up of three different individual layers and again
those layers are the zone of fibrosa zon of spongiosa and the zone of ventricularis and then surrounding it is going to be a nice little epithelial tissue called the endothelial lining all right all right that covers that part there now now that we have these uh valves separating these structures what's another important thing about these valves these valves are actually connected through these nice little collagen cords let's actually make these collagen cords here there's these nice little collagen cords here let me get the tricuspid valve out of the way here there's these nice little collagen
cords that are attaching to the cusps of the valves and they're they're nice little collagen cords and they're anchoring the valves in a nice taut position tight position normally okay so these little collagen like cords here are super super important what are these collagen cords here called these collagen cords are called cordate tendon so what are these cords here called they're called cord tendon and the tendon the cord a tendon are collagen cords and what is their purpose they're basically collagen cords that are attaching to the valves and keeping the valve flaps really nice and
tight to prevent them from uh back flowing up or actually ballooning back into the right atrium so this is important another thing is these cordate tendon how do we anchor them down how do we keep them nice and tight there's the muscle that actually kind of protrudes out from this area here and attaches to these cordate tendon so there's actually these nice little uh Peg like muscles that are pumping out here and attaching to these cordate tendon and these muscles are super super important because they're the ones that are anchoring these actual cord tendine down
which are anchoring these valves down what are these muscles here called these muscles are called your papillary muscles okay they're called your papillary muscles really really important the reason why is that when people get what's called Mis or heart attacks basically what happens is aeia occurs to these muscles and when they become uh es schic and maybe even start actually being affected severely because of that they can become weak and not able to contract if they can't contract they can't hold on to those cordate tendon nice and tightly so what starts happening to the valve
flaps they start becoming loose and whenever the right ventricle contracts it can push the valves back up okay and that can cause what's called a a valve regurgitation and that's that's not good that's really bad okay and but it's more common over here on the on the actual left side of the heart where the Bic cusp of the mitro valve is and just so that we're aware this one this valve here I'm going to just abbreviate it is the trir cuspate valve all right sweet deal that covers that now let's get into this part what
is this chamber here called what is this chamber of the heart here called this chamber of the heart is actually ref referred to since it's on the right side and it's the pumping chamber this is called the right ventricle so this is called the right ventricle very very important one okay now same thing over here on the left side you would still have those collagen cords let's say that I do the same thing here and I abbreviate my bicuspid valve here for just a brief moment here I put BV or MV because it can be
bicuspid valve or it could be mitro valve or you can even call it left atrial ventricular valve and just again what's that little recap here what are these little structures here called they're called your cordate tendon and the cord tendon are nice little collagen cords and they're anchoring the actual valves to these muscles here which are called the papillary muscles all right now the next thing is what is this chamber here called where the blood is actually coming down from the left atrium into this chamber right here this chamber here is called the left ventricle
this is the left ventricle very very important pump this is a very very powerful pump now now we get into the next thing the right ventricle will have to pump blood into this big old pulmonary circuit here so when it tries the pump blood into this pulmonary circuit it has to go through another set of valves what are these valves here called this valve right here is separating the right ventricle from the pulmonary trunk this is actually called your pulmonary trunk here so we call this and it actually looks like half of a moon so
it's a semi Lon right so they call it semi lunar but it's going from the right ventricle to the pulmonary trunk so it's called the pulmonary I'm going to abbreviate it semi lunar valve okay so this is called the pulmonary semi lunar valve now there's another one that's actually separating the left ventricle from the aorta and it looks like half of a moon so what do you think that one's called It's called The aortic semi lunar valve these are also very very important too okay so we have the pulmonary semi lunar valve separating the right
ventricle from the pulmonary trunk aortic semi lunar valve separ the life left ventricle from the orta these are important what is the purpose of valves it's to prevent the back flow of blood to provide a one-way blood flow all righty that covers that now what I need to do is I need to start going through the actual uh parts of the heart like actually a little bit more like thick structures wise so if you come right here you see how we're SE what separates the left ventricle from the right ventricle what is that big old
septum there called well it's separating the ventricles and it's in between them so it's called the interventricular septum so we call this bad boy right here if I were to kind of write it in between here they call this the inter ventricular septum so it's called the interventricular septum so the interventricular septum is separating the right ventricle from the left ventricle it's really really important that we have that barrier because if not the blood could be moved back and forth mixing the blood this is actually a common congenital disorder which occurs in the tetrology of
phet where they actually can have what's called a ventricular septal defect terrible terrible situation there okay now you can't see it it's hard to see because we have the pulmonary trunk in the aorta blocking it but there's another septum in between the left atrium and the right atrium it's called the interatrial septum okay just so that we're aware of that all right so now before we start going all the layers I want to hit just some of these great vessels that are coming off here real quickly so what is this guy here we said that
there's the pulmonary semi lunar valve separating the right ventricle from the pulmonary trunk so this whole big old Beast right here is called the pulmonary trunk now the pulmonary trunk comes up and splits into two nice good old arteries that are going to go to the lungs so this one here is going to be going on to the left side of the so they're going to the left lungs so they call this the left pulmonary artery this one over here is going to the right right lung so since this one's going to the right lung
this would actually be considered to be the right pulmonary artery the next thing the aortic semi lunar valve is separating the actual left ventricle from the aorta so when the blood is going up here it's going through the ascending aorta so this right here is called the ascending aorta and then we go up into this nice little arch called the aortic Arch now this is an important thing because if I were to label this right here the aortic Arch there's actually three important vessels that come right off of the aortic Arch and we're going to
go with them in order so the first one is called the brachio falic so this first one right here is called the bracho calic that's the first one right here okay the next one is going to be called another special one and this is called the left common cored artery so we're going to denote that lcca left common kateed artery okay and the last one is going to be What's called the left subclavian artery okay and just so that you're aware if you really are curious because I know that you guys are the brachio falic
is actually going to split into the into the right common cored artery so this splits into the right common cored artery and it also is going to split into another one called the right subclavian artery just say that you're wondering where the heck is the right one for these two guys okay that's where it's coming from and then again what will happen is eventually the blood from this aorta will continue and Go spread out to the multiple parts of the systemic circulation now let's cover the layers of the heart from inside all the way to
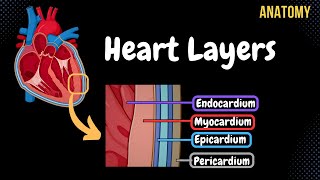
out all right so we imagine here that blood's going to be in these Chambers but what's lining the different parts of the heart so if you see this kind of like inner layer that maroonish layer right here this layer here is made up of an endothelial tissue okay so it's made up of like an epithelial tissue with a little bit of aerial or connective tissue underneath it this one right here is lining the inner layers of the heart so we call it the Indo cium so we call this layer the innermost layer the endocardium okay
then we go from the endocardium we go a little bit more out okay we go a little bit more out here and we get into this mid middle muscular layer right there this middle muscular layer right here is made up of nice cardiac muscle tissue it's a very very good cardiac muscle tissue and this cardiac muscle tissue that's the middle layer here this one is called The myocardium so it's called The myocardium and again what type of uh tissue is it made up of the tissue it's made up of is going to be cardiac tissue
so this is made up of cardiac tissue muscle cardiac muscle tissue all right very very important one now another little just kind of reference point here is when you're looking at the heart the left myocardium of the left ventricle as compared to the right myocardium of the right ventricle the left ventricular myocardium is much thicker because it has to pump blood for example the right ventricle only has to pump blood just to your lungs and back whereas the left ventricle has to pump blood all the way down to your little toe and then back up
right so you can imagine why this one has to have a thicker myocardium because it has to be a very powerful pump then we go into this outer blue layer this nice little teal layer here this teal layer right here is actually called has two names you can call it give it two names we can call it the epicardium or we can give it another name and I'll explain why we give it this other name in just a second another name that you can give it is called the visceral layer of the Cirrus pericardium you
guys are probably like I think I'm going to stick with epicardium I wouldn't blame you just giving you guys options of what the other names are the next thing here is we have a lot of fluid here in this little cavity here there's a lot of what's called this paric cardial fluid which this a nice Cirrus fluid here usually there's no blood or anything like that in this area here right under normal physiological conditions you just be a nice like Cirrus fluid this area right here is important because this is called the pericardial cavity this
is called the pericardial cavity so it's just made up of a nice Cirrus fluid now generally why is this important because in certain situations when there's actually going to be less fluid there can be more friction between this blue layer and this Green Layer and that's really bad because that can cause what's called pericarditis which is a very very severe pain that these people develop because of the friction that's rubbing up against between these two layers it's like a stabbing pain they say okay so it's again this is really important that allows for these two
layers to Glide up against one another during contraction and relaxation and prevent friction so a very important function of that pericardial fluid last one here this green layer is actually going to be what's called This is where this is why that's other name is really important here they call this the parietal layer of the Cirus pericardium so this is the continuous layer so for examp example I want to show you right up here you see how we have this blue layer here that's that epicardium or the visceral layer of the serus pericardium look how it
transitions you see how they're continuous with one another so it goes from here all the way to this one that's how it should be so normally you have a visceral layer covering the organ and a parietal layer covering the actual wall of that cavity okay in this case was the this paracardial cavity okay so that's the parietal layer of the serus pericardium now on the outer parts of it we have this brown layer and this Brown layer is so important this brown layer here is called the fibrous pericardium so it's called the fibrous pericardium super
super important structure it's actually made up of a what's called a dense fibrous irregular connective tissue so it's made up of dense irregular connective tissue super important there's actually three functions of the fibrous pericardium three important functions here one of the functions is it basically helps to Anchor the heart so it helps to Anchor the heart to the surrounding structures that's one function to Anchor the heart to the surrounding structures the other one is to protect the heart because it's a nice thick connective tissue it's going to provide a lot of uh protection to the
heart for any type of trauma or any type of damage or any type of other types of things that could actually cause the actual inner parts of the heart to be affected so it's good at protecting the heart because it's a nice thick connective tissue and because of this fibrous paric cardium the blood can't overfill with the actual uh blood the heart can't overfill with blood because whenever the heart is actually accumulating blood it can stretch well this fibrous paric cardium is not distensible it doesn't want to stretch so it prevents the heart from overfilling
with blood and over stretching that's an important function so it prevents heart from overfilling with blood right so that's another function so this is the function of the fibrous pericardium okay three very very important functions anchors the heart to the surrounding structures protects the heart and prevents the heart from overfilling with blood so that covers that one now in this we've actually talked about all the different layers and I just want you to understand one other thing that just because I did it for these ventricles it's the same for all the other chambers of the
heart now another thing here is that if you look here for the mitro valve or the bicuspid or the ortic semilunar valve they're also covered with that nice endocardial lining okay so Niners we have pretty much covered everything that we're going to need to know here for basically the anatomy and the histology of the cardiovascular system I really hope it made sense I really hope that you guys did like it if you guys did please hit the like button comment down in the comment section and please subscribe as always engineered until next time
Related Videos

48:01
Cardiovascular | Electrophysiology | Intri...
Ninja Nerd
1,624,174 views

18:32
Cardiovascular | Anatomy of the Heart | He...
Ninja Nerd
2,291,450 views
Alpha Waves Activate 100% of Your Brain Af...
Relaxed Mind

8:52
Circulatory System | Pulmonary Circulation
Ninja Nerd
703,301 views

23:59
Cardiovascular | Cardiac Cycle
Ninja Nerd
1,686,880 views

16:31
How to Stop Procrastinating and Finally Ta...
Ali Abdaal
220,922 views

Deep Focus - Music For Studying | Improve ...
Greenred Productions - Relaxing Music

15:20
Heart Anatomy: Chambers, Valves, & Structu...
RegisteredNurseRN
45,645 views
11:21
Anatomy of the Heart (Layers, Conducting S...
Taim Talks Med
195,942 views

11:17
Circulatory System | Coronary Circulation
Ninja Nerd
590,533 views

44:59
Cardiovascular | Cardiac Output
Ninja Nerd
1,336,821 views

14:26
How the Heart Works (Animation)
Thomas Schwenke
185,180 views

1:12:50
Embryology | Development of the Heart ❤️
Ninja Nerd
1,196,991 views

17:46
Heart Conduction System & ECG (EKG)
Siebert Science
152,116 views
7:50
Cardiac Action Potential, Animation.
Alila Medical Media
2,628,865 views

15:29
Coronary circulation of the heart
The Noted Anatomist
1,661,525 views

8:43
The Cardiac Cycle is SO EASY! Stop Making ...
Interactive Biology
1,263,113 views

13:06
Blood supply to the brain
The Noted Anatomist
1,026,806 views

28:32
The Cardiovascular System: An Overview
Strong Medicine
767,618 views

1:19:14
EKG Basics | How to Read & Interpret EKGs:...
Ninja Nerd
2,792,592 views