Metabolismo de Lipoproteínas
121.72k views2300 WordsCopy TextShare

Victor Cilleros
METABOLISMO DE LIPOPROTEINAS
Repartir lípidos entre los órganos que los necesitan es todo un desafí...
Video Transcript:
Foods with olive oil and fat, in moderation, in addition to being tasty, provide us with a lot of energy and are a source of vitamins and essential fatty acids. But delivering lipids to the organs that need them is a challenging task, because they are insoluble in water and do not circulate well through the circulatory system. To fix that, the human body has developed lipoproteins.
Lipoproteins are spherical macromolecules which transport lipids through the bloodstream. On the outside they consist of a monolayer of phospholipids and cholesterol and on the inside they mainly transport triglycerides and cholesteryl esters. Around this structure, there are apolipoproteins, proteins whose function is to maintain the structure and to act as labels, indicating what actions must be carried out, for example loading lipids, unloading lipids, or activating certain enzymes.
The name of each apolipoprotein is given by the prefix "Apo-" followed by a letter. In this video we will talk about the proteins Apo-A1, ApoB-48, ApoB-100, ApoC-2 and ApoE. There are three pathways of lipid transport.
The exogenous pathway, the endogenous pathway and the reverse pathway. The exogenous pathway distributes dietary lipids from the intestine to various tissues, including the liver. The endogenous pathway goes from the liver to the extrahepatic tissues.
And finally, the reverse pathway transports lipids from these tissues back to the liver, where they can be excreted from the body. Each pathway uses a specific lipoprotein. In general, lipoproteins start their journey loaded, with a large size and, as they distribute lipids, they become smaller and denser.
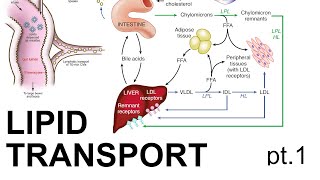
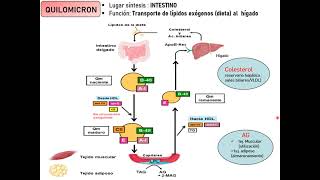
Depending on their size, they receive a name that tells us where they are on their pathway. The exogenous pathway receives this name because it transports lipids from the diet, considered "exogenous" or "from outside. " This pathway begins by collecting lipids in the small intestine and sends them through the circulation with a lipoprotein called chylomicron.
After distributing lipids to various tissues, the remnant chylomicrons reach the liver, which finally removes them from the circulation. The exogenous pathway begins with the digestion of lipids. This is quite a challenge, as they are hydrophobic molecules that do not mix well with the water-based fluids in our body.
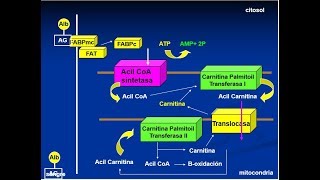
To digest them, the solution is to wrap the lipids with bile salts. These are amphipathic molecules similar to cholesterol, half hydrophobic and half hydrophilic, which help divide the lipids into small pieces and facilitate the action of enzymes. The most abundant lipids in food are triglycerides and cholesteryl esters, although there are others such as phospholipids or certain vitamins.
In the intestine, triglycerides are digested with pancreatic lipase, which cuts and produces fatty acids, diacylglycerol and monoacylglycerol. On the other hand, cholesteryl esters are hydrolyzed with the cholesteryl sterase, which produces free cholesterol and a fatty acid. Once broken into smaller parts, these molecules can then be taken up by the intestinal cells, the enterocytes.
To deliver lipids into the circulation, the enterocytes must rebuild the triglycerides and cholesterol esters and introduce them into the lipoprotein chylomicron. Enterocytes and other cells can synthesize triglycerides through two metabolic pathways. The monoacylglycerol pathway, which begins with a monoacylglycerol to which two fatty acids are added with two acyl-transferase enzymes; and the phosphatidic acid pathway, which starts with a glycerol-3-phosphate and adds three fatty acids to it.
On the other hand, cholesteryl esters are synthesized with the enzyme acyl-CoA: cholesterol acyl-transferase or ACAT, which binds a fatty acid to a free cholesterol. Once the enterocytes have rebuilt the triglycerides and cholesteryl esters, they introduce them into the chylomicrons and release them to the lymphatic system. First, chylomicrons are released into a duct in the center of the intestinal villi called the lateal duct.
From there, chylomicrons travel through the lymphatic system until they reach the bloodstream. The newly synthesized chylomicrons are the largest lipoproteins that exist and initially they only have ApoA-1 and B-48. ApoB-48 is unique to chylomicrons and it's important because it serves as a marker.
Once in the blood, chylomicrons receive Apo-C2 and ApoE from HDL, another type of lipoprotein, and in return they transfer ApoA-1. The function of ApoC-2 is to activate the Lipoprotein Lipase or LPL, an enzyme expressed on the surface of the endothelium, the cells that recover the inner side of blood vessels. While chylomicrons are in circulation, LPL hydrolyzes their triglycerides and releases fatty acids.
These diffuse through the medium and are taken up by cells near the vessel, often muscle or adipose tissue. Muscle cells use fatty acids for energy, whereas fat cells store them as triglycerides. After delivering the majority of triglycerides, chylomicrons lose ApoC-2 and are called 'remnant chylomicrons'.
Remnant chylomicrons have ApoB-48, ApoE and are rich in cholesteryl esters. To eliminate them, the hepatocytes take up ApoB-48 with the LRP receptors and the heparin sulfate proteoglycans. Furthermore, they can also bind ApoE with LDL receptors.
Thanks to these receptors, the hepatocytes endocyte the remaining chylomicrons and eliminate them from the plasma. Finally, the liver will use the cholesteryl esters taken, to synthesize the bile salts, which will facilitate the absorption of lipids in the next digestion. The exogenous pathway is a very profitable source of energy from the diet and is therefore regulated by the hormone insulin.
This hormone is released by the pancreas after each intake and it promotes energy storage. On the one hand, insulin increases the activity of endothelial LPL, making it easier for chylomicrons to distribute fatty acids and adipocytes to take them up. Furthermore, insulin also acts on adipocytes, promoting the release of the glucose transporter GLUT4 on their surface.
Glucose is then used by adipocytes to synthesize glycerol-3-phosphate and to make triglycerides via the phosphatidic acid pathway. The endogenous pathway receives its name because it carries internal or endogenous lipids. This pathway begins in the liver and distributes lipids to extrahepatic tissues.
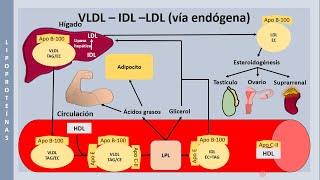
The lipoproteins in charge are VLDL, which, after distributing lipids, become IDL and LDL. To send lipids from the liver, hepatocytes introduce triglycerides and cholesterol to the ApoB-100 apolipoprotein, generating 'Very-Low-Density Lipoprotein', or VLDL. VLDLs are released into the circulation and begin their journey to distribute lipids throughout the body.
In the early stages, they receive ApoC-2 and ApoE from HDL. ApoC-2 activates the endothelial LPL, which cuts triglycerides and releases fatty acids in extrahepatic tissues. After losing these less dense lipids, they become 'Intermediate Density Lipoproteins' or IDL, richer in cholesterol and without ApoC-2.
IDLs return to the liver in two ways. Half of the IDLs are taken up by hepatocytes with the LDL receptor, which binds ApoB-100 and ApoE. The other half of the IDL gets is processed by the hepatic lipase, which doesn't need ApoC-2 and releases fatty acids.
In the first case, IDLs are endocytized and disappear from the bloodstream. But in the second case, IDLs remain in circulation only with very few triglycerides, reduced in size and without ApoE. This turns them into 'Low-Density Lipoproteins', or LDL, very rich in cholesteryl esters and with ApoB-100 as the only apolipoprotein.
But how is cholesterol distributed throughout the tissues? LDLs have a quite long half-life, and are metabolically stable during three days. During this period, they are endocyted by various tissues with the LDL receptor, which binds ApoB-100.
Most cells express LDLRs, but the uptake is especially active in those organs that use cholesterol for biosynthesis, such as the liver, to synthesize bile salts, the adrenal glands, to synthesize aldosterone or cortisol, the ovaries, to generate estrogens , or oligodendrocytes, to make myelin. These tissues and others are responsible for collecting and eliminating LDL from the circulation. Therefore, in healthy conditions, these tissues are the final destination of the endogenous pathway.
The endogenous pathway has control points that guarantee a sufficient supply of cholesterol and prevent an excessive accumulation. The key to this regulation is the intracellular cholesterol esters themselves. When their concentration is low, they activate mechanisms to capture more LDL and when their concentration is high, they close the entry of more cholesterol.
One regulatory mechanism is the SREBP2, SCAP, and INSIG system. These are three proteins of the endoplasmic reticulum. When there is not enough cholesterol, SREBP2 and SCAP are liberated from INSIG and migrate to the Golgi apparatus.
There, two proteases cut SREBP2. The released fragment translocates to the nucleus and activates the transcription of several genes, including LDL receptors to capture the more cholesterol and restore proper levels. In the opposite case, when there is too much cholesterol, this molecule retains the three proteins in the endoplasmic reticulum, which inhibits the synthesis of LDL receptors (among other genes) and no more cholesterol is taken up.
In addition, free cholesterol also promotes its own storage, increasing the synthesis of the enzyme ACAT, which generates cholesterol esters that can be stored in deposits in the cytosol. If there are too many LDL and not all of them can be taken up, the time were they are stable can be exceeded. Then, the LDL lipids and ApoB-100 can suffer oxidation, becoming oxLDL.
The cells responsible for eliminating oxidized LDL are the macrophages near the vessels known as supbendothelial macrophages. These cells capture and phagocyte oxidized LDL with their receptors, called Scavenger Receptors. In pathological conditions such as hypercholesterolemia, LDL cholesterol levels are chronically elevated; and macrophages take up excessive amounts of cholesterol.
This is because, unlike LDL receptors, scavenger receptors are not regulated by product. This causes macrophages to store excessive amounts of cholesterol, generate atheroma plaques and start atherosclerosis processes as the pathology progresses . The reverse pathway receives this name because it's the only one that transports lipids in the opposite direction: from extrahepatic tissues to the liver, collecting excess cholesterol to excrete it in the form of bile salts.
The lipoproteins in charge are HDL or high-density lipoproteins. Contrary to what it seems, HDL is not generated in extrahepatic tissues, but instead is synthesised by the liver and the intestine, travels throughout the body capturing cholesterol and then returns back to the liver. As they fill up with cholesterol, HDL goes through four stages: ApoA-1, pre-β-HDL, HDL3, and HDL2.
First, the liver and intestine synthesize ApoA-1, which enters the circulation and targets extrahepatic tissues. ApoA-1 collects cholesterol by interacting with the proteins ABCA1 and ABCG1, which export cholesterol from cells using ATP. As they accumulate free cholesterol and phospholipids, ApoA-1 turns into nascent HDL, called pre-beta-HDL because of the way it migrates in a gel.
Because it still has few cholesterol, it has a flat or disc shape, which is why sometimes it is classified as 'discoidal HDL'. While in circulation, ApoA-1 activates the enzyme Lecithin Cholesterol Acyl Transferase, or plasma LCAT, which esterifies cholesterol with fatty acids. Cholesterol esters are more hydrophobic than cholesterol, so they enter inside the interior of the lipoprotein, which increases and acquires a more spherical shape.
Therefore, the action of LCAT fills in the discoidal HDL and transforms them first in HDL3 and later in HDL2, both known as spherical HDL or alpha-HDL, because of the way they migrate in a gel. The main function of HDL2 is to deliver cholesterol to the liver. However, they also serve as a reservoir for ApoC-2 and ApoE, lending and receiving them from other lipoproteins such as chylomicrons and VLDLs.
HDL2 delivers cholesterol to the liver in two ways: directly and indirectly. Directly, HDL2 binds to the hepatic SR-B1 receptors and delivers cholesterol esters to the liver. Indirectly, HDL transfers its cholesterol to other lipoproteins for them to deliver it.
This occurs thanks to the 'Cholesteryl Ester Transporter Protein' or CETP, a plasma protein that exchanges HDL cholesterol esters for VLDL triglycerides or chylomicrons. Hence, it will be VLDL and chylomicrons, at the end of their path, the ones that deliver cholesteryl esters to the liver. On the other hand, HDL2 enriched with triglycerides are processed by hepatic lipase, which does not need ApoC-2, and after getting emptied, they become HDL3 again.
Unlike LDL and its LDL receptors, HDL2 discharge cholesterol without endocytosis, so they remain in the circulation emptied and ready to continue collecting more cholesterol from extrahepatic tissues. This generates a constant HDL recycling, between HDL2 large and full of cholesterol, and HDL3 smaller and empty. And.
. . that's it!
Lipoprotein metabolism is difficult to remember, especially because of the diversity of apolipoproteins and their different functions. So, to help memorize you can use the following mnemonic rules. ApoA-1 is in chylomicrons and HDL, but its main function is in HDL.
So a trick to memorize it might be to think that HDL are the "good cholesterol" and that they always get "excellent grades, all A's". That way, we could remember that ApoA-1 goes with HDL. We can use the A to remember that its function is to 'Acquire cholesterol and 'Activate the LCAT.
To remember the function of ApoB-48 and B-100, B-48 is from chylomicrons and B-100 from VLDL and LDL, we can remember that B-48, "forty eight" sounds a bit like "food" and that B-100 is a "100 year old" man with lots of "bad" LDL cholesterol. The following are ApoC-2 and ApoE, which go hand in hand in all the pathways, both being in chylomicrons, VLDL and HDL. We can remember the function of ApoC-2, with the "C" for "cutting", because it "cuts" triglycerides, since its function is to activate the endothelial LPL.
And for ApoE, we can remember its function with the "E" for "Entregar (deliver)" to the liver. Since its function is to bind to the LDL receptors and help capture lipoproteins. And.
. . that's all!
If you liked the video and you'd like to support me, you can leave a like or subscribe. And if you have any suggestions, or other tricks to remember, I read you in the comments! PS.
Heyyy! cheers up with your study, you got this!
Related Videos

18:28
Metabolismo de las Lipoproteinas
Dr. Luca Merlini
518,666 views
35:33
Metabolismo de las lipoproteínas, clasific...
MIPSITO NOE RUIZ ZAPATA
16,166 views
20:35
Digestión y absorción de lípidos
Instituto Mortaji
6,748 views

20:34
PERFIL LIPÍDICO VALORES NORMALES | GuiaMed
GuiaMed
165,058 views
18:57
Don’t Worry About “Bad” Cholesterol, Says ...
The Minimalists
1,039,523 views

1:03:35
Metabolism | Lipoprotein Metabolism | Chyl...
Ninja Nerd
1,204,668 views
![Lipoproteínas: Quilomicrones, VLDL, LDL y HDL [Transporte de lípidos]](https://img.youtube.com/vi/3qbZwjH_nac/mqdefault.jpg)
8:22
Lipoproteínas: Quilomicrones, VLDL, LDL y ...
Metabolismo
258,648 views

12:56
Intro to Lipids & Lipoproteins: Why there ...
Peter Attia MD
765,387 views
![Catabolismo de ácidos grasos [Movilización, activación y beta oxidación] | Bioquímica](https://img.youtube.com/vi/xQuW745Sj10/mqdefault.jpg)
8:11
Catabolismo de ácidos grasos [Movilización...
Metabolismo
139,768 views

6:37
METABOLISMO DE LIPIDOS PARTE 1
Bioquimica Virtual UBA
150,724 views
14:17
Lipid Transport (pt. 1)
Dirty Medicine
399,908 views

19:44
🔥BETA OXIDACION de los ACIDOS GRASOS!! (F...
Profesor Matias Rodriguez
158,409 views

14:58
LIPIDOS
Bioquimica Virtual UBA
139,537 views
![[SPANISH] The Complement System (Activation, Pathways and Regulation)](https://img.youtube.com/vi/OfHridOac2A/mqdefault.jpg)
7:16
[SPANISH] The Complement System (Activatio...
Victor Cilleros
187,870 views
1:02:04
Bioquímica | Colesterol | Metabolismo de l...
Instituto Mortaji
99,613 views
22:29
Seminario Metabolismo de lipoproteínas. P...
Química Biológica Cátedra 1. FMED-UBA
10,923 views
![Metabolismo de la LDL [Origen, función y captación por endocitosis] | Bioquímica](https://img.youtube.com/vi/yDtPSAV3QlM/mqdefault.jpg)
11:12
Metabolismo de la LDL [Origen, función y c...
Metabolismo
38,756 views

17:11
Lipoprotein metabolism and transport | Chy...
Animated biology With arpan
313,655 views
14:47
El metabolismo de los lípidos, sus alterac...
Fundación redGDPS Diabetes
42,640 views
1:24:43
BIOQUIMICA GRASAS lipólisis y betaoxidació...
Dr. Roosvell Pairazamán
86,304 views