Respiratory Failure | Clinical Medicine
61.55k views5633 WordsCopy TextShare

Ninja Nerd
Premium Member Resources: https://www.ninjanerd.org/lecture/respiratory-failure
Ninja Nerds!
Profes...
Video Transcript:
what's up Ninja nerds in this video today we're going to be talking about respiratory failure this is a part of our clinical medicine section if you guys like this video it helps you please support us and you can do that by hitting that like button commenting down the comment section and please subscribe another way that you can really help us but also help yourself is go down the description box below there's a link to our website where I really suggest and really push you guys to become a member because there we have a lot of
awesome things we have notes illustration question Banks we're developing exam prep courses for those of you who are taking your boards and we even have some merchandise there that I suggest you guys check out all right without further Ado let's talk about respiratory failure so with respiratory failure what is the primary way that these patients present they can look a lot of different ways and that's why we're going to talk about all these different types of causes of respiratory failure but often times one of the most common ways that we look at patients who have
respiratory failure is based upon their oxygen saturation so when they come into the hospital or they go into the clinic they get one of those monitors that goes on their finger and it gives you an spo2 and when that SP2 is rather low we can potentially suggest that this patient is exhibiting signs of respiratory failure and then we'll go through the causes of that now I want you to understand some basic physiology nothing crazy you need to know that whenever these patients have problems generally there's some type of gas exchange process that is occurring between
the lungs and the pulmonary capillary bed that blood after it's exchanged will then move into the left atrium when it moves into the left atrium then go into the left ventricle from the left ventricle do then get pumped out into the arterial system and when it gets pumped out into the arterial system we can then test that by doing like arterial blood gases or putting the Probe on the finger which gives us a percent saturation so whenever you have a patient who exhibits a low let's say amount of oxygen within the bloodstream what do we
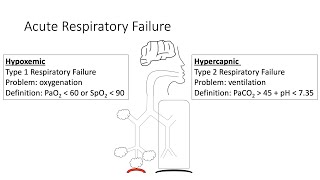
call that whenever you have low oxygen within the bloodstream this is called hypoxemia so it's low oxygen within the bloodstream and now this can be measured in a couple different ways one is you can measure it via that pulse oximeter and the way that we look at that is we say oh the patient has a very low spo2 or we get an ABG that tells us that they have a low sao2 or a pao2 and i' say the latter one is the more common one that we go off of so if patients have low sp2s
low SA o2s or low p2s these are other ways that we can quantify a patient having hypoxemia the question arises what's a low spo2 it can V vary from person to person Patient to Patient but on average we say something less than 90% And then for the pao2 we go to the range of a patient having something less than 60 mm of mercury so I'm going to put less than 60 mm of mercury these are the ways that we can quantify a patient having hypoxemia which may Define their respiratory failure we just have to figure
out why is there this problem within the lungs where gas exchanges occurring between the pulmonary capillaries so let's go through that the first reason one of these patients can develop hypoxemia is called a VQ mismatch now when patients have VQ mismatch the primary problem is they have poor ventilation to their alvioli we've already talked about this in great detail in pathophysiology but concept here is something in some way shape or form there is poor ventilation maybe the alveoli is filled with a little bit of pus or fluid and in that scenario you can't get the
amount of oxygen molecules to go into this alveola as you usually would if this thing didn't have that material you wouldn't have a problem or if there was something kind of like within the Airways that were kind of like mildly obstructing the airway these are Concepts where ventilation is now going to be poor to this alveoli and same thing look at this alveoli over here this sucker's collapsed am I going to get good ventilation to this alvioli no so the concept here is that these patients are going to get poor ventilation but the amount of
blood flow moving through the pulmonary capillaries in these patients is normal that's why there is a mismatch it should be normal and normal so if I have normal what we call Q perfusion and decreased ventilation this is what causes the mismatch if there's poor ventilation there's not enough oxygen molecules getting into these alveoli I won't be able to move the oxygen the amount that I want to into the alveoli from from the alveol into the pulmonary capillary blood and so when the blood leaves here as it moves through what's it going to show it's going
to show a low oxygen concentration and that can be via these things that we just talked about but you have to ask yourself the question what is this process here well this process here where we have low vent pation could be due to alveolar filling so the alveoli are filled filled with what it could be a bunch of different things it could be they're filled with pus and the scenarios of pneumonia it could be they're filled with fluid like in pulmonary edema it could be that they're filled with h blood like an alveolar Hemorrhage so
if you understand that they're filled with something that's reducing the vent vation to that Alvi then you have a very strong concept of why ventilation would be reduced so there's increased alveolar filling reducing the ventilation to that alveoli and therefore less gas exchange what about in this scenario the alveoli is collapsed so there's increased alveolar collapse what is it called whenever the alvioli collapse that's called atelectasis so if a patient exhibits atelectasis and there's many different reasons for atacas is it could be they're not taking a good enough deep breath in it could be um
that in this particular scenario they have something that's pushing down on their alvioli like fluid like a plural Fusion or numo thorax or there could be some mucus within the Airways either way these are concepts of where you're going to have VQ mismatch and then for hypoxemia one big thing and these patients I really need you to remember this for VQ mismatch they have a normal or elevated they usually more often than not an increased what we're going to call minute ventilation which we express as ve meaning these patients often breathe really fast so they
usually have increased respiratory rates and increased work of breathing usually as a response of their hypoxemia they're like hey man oxygen isn't good I got to breathe faster and deeper and so often times more than not these patients will breathe super super fast and really work hard and take deep breaths in and that'll often cause you to clear a lot of CO2 so often times these patients CO2 tends to be low or maybe just on the lower limit of normal and that's important to remember here what about the other scenario where the ventilation is actually
normal or maybe even a little bit increased but the perfusion stinks so that's another scenario here so now I have a patient who has poor perfusion maybe it's because these puppies are clamped down or maybe there's a clot right here that is present Within These vessels but either way maybe the clot is not completely uding the flow but there's a little bit of flow coming through there but it's very very little now ventilation in these alveoli is there anything filling them or do they look collapsed no so if that's the case then this is normal
this is reduced so ventilation will be normal you'll be able to get a good amount of air here you'll be able to allow for some gas exchange to occur here but it's going to be very little there's little blood that's squeezing through this area to pick up the oxygen and so because of that you're not going to be picking up as much oxygen because you're not getting as enough blood flow to the area so these patients will also drop their oxygen in the form of an O2 saturation an sao2 or a pa2 what's the cause
for the low perfusion pulmonary vase or constriction or a pulmonary embolis I'd say by far it's going to be pulmonary embolism and the rare scenarios it could be some type of it could be some type of extense pulmonary vasal constrictive mechanism but here's what I want you to remember comes patient comes in hypoxemia if they have hypoxemia think about VQ mismatch either a ventilation or a profusion problem same thing exists though over here where these patients will also potentially because of their hypoxia they will usually have increased respirations increased work of breathing so they will
blow their CO2 two down sometimes patients with pulmonary imali will have some degree of increased Dead Space so they could potentially have their CO2 a little bit more normal than usual all right that's VQ mismatch the next reason of why is going to be a patient who developed something called hyperventilation now this is really really important that you get the point here these patients do have a low minute ventilation so they have a very low ve minute ventilation now what that means is is that their respiratory rate is either super super low and they're not
breathing at all or breathing really really slow or their tital volume which we represent as VT is really low they're taking very shallow breaths if that is the case that would be the primary reason why these patients don't bring enough oxygen in and get enough CO2 out that is the big big concept here so what I want you to understand is in both of these scenarios you know what the big overarching theme is is ventilation is reduced so they don't get Co2 out and they don't get oxygen in so these patients will have both a
low O2 and a high CO2 potentially so they may have a high CO2 and a low O2 this is the big thing to remember about hypoventilation hypoventilation is one of those that can cause elevated CO2 and maybe a normal or even decreased oxygen question comes why are they hypo ventilating why are they not getting enough oxygen coming through their big Airways and into the small Airways there's no VQ mismash there's no pus or fluid or any kind of alveolar collapse it's just they're not taking deep enough breaths or they're not breathing fast enough so the
amount of air that they're moving into these air columns is reduced therefore less oxygen and less CO2 being cleared if that happens that's why they build up what's the causes make it super simple go back to physiology you have a respiratory Center it sends signals to your actual muscles to your nerves that go to the muscles cause them to contract diaphragm contracts intercostals retract you take deep breaths in and you exhale but the rate at which you breathe is determined by the respiratory Center so if I have CNS depression let's say I jack this thing
up so if I have CNS depression as one potential cause here what's that going to do to my respiratory rate that's going to drop my respiratory rate and if I drop my respiratory rate I drop my ventilation and I accumulate CO2 and I potentially don't get enough oxygenation so now that's going to be one of the problems why am I depressing the CNS one is a cerebrovascular action you stroke out this area or more common is usually drugs so drug overdose there is many different types of drugs but I'd say the big ones to remember
here are going to be opiates so if someone takes way too many opiates or they take way too many benzos and they overdose on these all right if that happens they have a decreased respiratory rate decreased signals decreased exertion of the muscles what if I damage the nerves or I damage the muscles and they don't contract if they don't contract I can't take a deep breath in that lowers my tidal volumes lowers my minute ventilation same concept neurom muscular dysfunction would be another big one and again what's the overarching theme with this one that it's
going to drop my tital volumes sick now if that happens I don't take deep breaths in I accumulate CO2 and don't oxygenate what's causes here one is called Gom Beret syndrome another one is called spinal cord injuries another one could be like myasthenia gravis another one could potentially be muscle exhaustion or fatigue these are Big causes so if I damage my spinal cord I damage potentially my I demate my neurons or I cause neuromuscular dysfunction or I weaken the muscles that's all going to cause them to not take deep breaths last but not least what
if I obstruct the airway and I can't get Co2 out and then my lung's hyper inflate oh that's interesting right so the last one could be Airway obstruction if a patient has Airway obstruction and in some other scenarios it could just be airway disease what this does is it does something super weird they actually breathe fast but their lungs become hyperinflated and they can't take in deep breaths so what happens happens to their title volume it drops this is classic and I mean classic of patients who have exacerbations of reactive airway disease so this would
be an acute exacerbation of their COPD um COPD or it could be an asthma exacerbation these are super common because they'll cause so much Broncos spasm you can't get air out so they hyperinflate the lungs are so big they can't take a deep breath in these are all mechanisms here this is the one that I really want you to remember where all the other ones will probably blow down their CO2 this is the one where you'll probably rise your CO2 okay come to the next one we come to the severe Guys these are the patients
who are like refractory hypoxics this is usually what we call an extreme low VQ mismatch so we call this a pulmonary shunt this would be a patient who has one of these things up here but the worst case scenario imagine I take this entire alveoli and I fill it with fluid or pus so in this particular scenario I have the worst case I have severe alveolar filling if I fill these puppies to the absolute Brink that is a big big problem so if I have severe alveolar filling I'm going to get literally what kind of
ventilation to this you can you get any air into this thing no no ventilation what if this puppy collapses completely can I get any air into this one pretty much no so if I have a patient who has severe alveolar color collapse or severe alveolar filling the process that happens here is that they get no ventilation that occurs here so I'm trying to get air that comes down here but that's blocked or I have something that's uding this Airway or causing it to collapse that's blocked off I won't even ventilate these dang things so therefore
gas exchange doesn't even occur this process here is inhibited and even though the perfusion is actually maintain a relatively normal blood is just going to flow on right through here with almost no gas exchange whatsoever so what happens to the pa2 here or the SP2 drops so these patients have extremely low oxygen levels all right question then comes again same thing what's causing this severe alveolar filling this is very very common of patients who have what's called a DS I'd say it's probably one of the biggest ones another one could be if they have severe
pneumonia like really really bad pneumonia or severe edema severe pulmonary edema can also do this or if they have like diffuse alveolar Hemorrhage it's just the worst case scenario of these things that's really the primary trigger here okay the last one is if the alveolar collapse so they have intense alveolar collapse like the worst case scenario so this is like the most severe atelectasis that you can think of if their alveola collapse is intense this is usually two things it's usually severe atelectasis or it's a proximal mucus plug so a big plug somewhere within the
Airways that they get no air flow so this would be a mucus what we call mucus plug these are two big reasons of why patients can develop a increased Alvar collapse no ventilation no gas exchange severe hypoxemia again these patients will usually have increased Mena ventilations they will breathe pretty dang fast because they're trying to improve their oxygenation so their respiratory rates will go up their work of breathing will go up they'll look like hot crap and because of that they will sometimes blow their CO2 down to normal or they will completely drop their CO2
same thing for the extrapulmonary shunts these patients same thing they'll probably increase their minute ventilation what's different between a pulmonary and an extra pulmonary shunt the the blood flow isn't just bypassing in the pulmonary arteries it's bypassing outside the pulmonary arteries so the best example of this is that blood is usually oxygenated blood will move to the left heart right from the lungs so this should be rich in oxygen this whole thing here but if for whatever reason I splint open a hole between the heart and deoxygenated blood diverts over into the oxygenated blood and
I have blood to go from the left atrium left ventricle into the arterial system I test it what am I going to find deoxygenated blood so if I were to imagine here blood's coming out of the heart what am I going to see as the O2 it's going to be low because I'm mixing blood here they're going to have crazy low O2 levels now what's the reason for this the reason is there's some type of cardiac shunt and this is usually two examples here one is the patient has what's called a atrial seal defect they
have a PFO or they have a vssd and what happens is the blood is shunting across these holes within the heart but this cardiac shunt has to be under high pressure the right heart pressures have to be high enough to push blood over to that side the only thing that would do this is you'd have to have a cardiac shunt and the patient would have to have pulmonary hypertension so they would have to have pulmonary hypertension in the presence of a cardiac shunt for the pressure to be high enough to shunt the blood over that
is the big difference here between these po patient populations there is another Rarity called pulmonary avms but I don't want to take too much time with that the last concept to understand here is in these patients that come in with hypoxemia it is really really important that you kind of use different tests so if you test them and look at their SP2 you look at their ABG another thing is giving them 100% oxygen when you give them 100% oxygen it takes a look to say which one of these would correct and so that's the big
thing here so with VQ mismatches you give them 100% oxygen they will improve cuz some of their alvioli are healthy they're well well ventilated some are well profused hypoventilation you give them more oxygen they actually will improve but these you give them oxygen they have almost no good alveoli or good profusion here this is going to literally not change with oxygen all right now that we've covered this let's move into the diagnostic process of respiratory failure all right so now we have to learn how to diagnose respiratory failure so we're going to go through and
say okay how's Z how do I determine if there's a type one how do I determine if there's a type two respiratory failure I don't really know that stuff so let's go through it so first thing is look for the patient who appears to be in respiratory distress that might be one particular sign they're breathing really really fast at 30 breaths per minute they're using accessory muscles they're using nasal flaring they have intercostal retractions they don't look good look at their vitals what does their O2 saturation suggest is it less than 90% they may have
hypoxemia and so then I got to get an ABG because I think the ab is going to help me to determine is this a type one or a type two I know that in type one you have to have a low pao2 and again that has to be less than 60 in type two you have to have an elevated Pac CO2 generally greater than 45 or greater than 50 and it doesn't really matter what the pa2 is for that one it can be low but I I just have to be able to differentiate because that's
going to tell me if it's hyperventilation or it's going to tell me if it's a VQ mismatch shunt or diffusion capacity problem so that's right away the thing I'm going to do if I obtain it and I see a pco2 of greater than 45 I know it's hyperventilation so then I got to go and think is it a CNS depression issue is it neuromuscular failure or is it a COPD or asthma exacerbation and that's that's where the history comes into play and other tests if that is not the case and the pco2 is normal or
decrease then I know it's not hypoventilation it's got to be something else now really quickly they'll say okay do 100% oxygen but before you even do that one of the big things that can be helpful is that there's only one of these that's called the decreased diffusion capacity which we see in I usually this is the only one that will happen with exertion so if you get the patient up you start walking them around the the unit and they start having you know decreased oxygen saturation or they have a low pao2 on their ABG after
you walk them that would be suggestive of an impair diffusion like an i disease but we're going to go to the shunt and the VQ mismatch you give these patients 100% oxygen this is really the test if you give them 100% oxygen and the hypoxemia does improve so their SP2 goes up or you get an ABG afterwards and it goes up that's suggestive of a VQ mismatch because there's some ventilation that's getting there so then you got to think okay from the VQ mismatch which one could it be well how do I really determine that
get a lot of different tests get some chest Imaging get a chest x-ray get a chest CT it'll look for a lot of these problems it'll say is it atelectasis is it pneumonia is it pulmonary edema is it some type of mucus plug or is it a PE that I do a CT pulmonary andram to prove hypoxemia does not correct it's a shunt so it's likely a shunt and you have to determine is it a true like pulmonary shunt or is it a true intercardiac shunt and so often times I just would get an echocardiogram
an echocardiogram would help me to say say oh there's an ASD there's a PFO there's a vssd and I can see the blood passing across from the right to the left and if the echo isn't the answer you can also get chest damaging to make sure that you rule out a severe atelectasis you rule out ards you can rule out severe pneumonia things to that effect so it's really important after that to find out a little bit more about the etog all right so we have a patient who has respiratory failure you want to be
able to treat these patients appropriately and so there's different ways that we can do this one of the ways that we can do this is non-invasive ventilation one of the best methods I like to use in patients who have a lot of pulmonary secretions and they're hypoxemic is usually high flow nasal canula and you can give them a lot of F2 and you can give them a lot of volume of air that rushes into the lungs and it helps with kind of mu mucocin is moving a lot of secretions out especially in pneumonia and it's
also good in patients who um have very low oxygen levels this is a really good one in patients who maybe have a different scenario where they may require something called by Lev positive airway pressure also is BiPAP there's two really big scenarios that I want you guys to remember for this one one is if they have hypercapnic respiratory failure so this is your type ones if they have the type one I'm sorry these are the type two respiratory failures I apologize for the type two respiratory failures where the CO2 is really really elevated this is
the type of you know kind of non-invasive ventilation that you'd want to perform another one is cardiogenic pulmonary edema if a patient has CHF they have a lot of pulmonary edema in their lungs BiPAP is actually really good to reduce the work of breathing and also reduce the actual pulmonary edema via that high amounts of Peep and it also will improve cardiac output so BiPAP is good in these particular scenarios for type 2 respiratory failure and cardiogenic pulmonary edema high flow is good for oxygenation especially in a patient with a lot of pulmonary secretions and
hypoxemia now if a patient fails non-invasive ventilation often times what will go to is endot tral tube intubation and this is usually going to be in refractory respiratory failure in other words we've tried highlow nasal candy oxygenate them we've tried BiPAP to reduce their work of breathing we've tried all the therapies to treat the underlying cause they're still refractory then you may have to intubate them that leads to the next step if I have a patient on the ventilator how the heck am I supposed to know how to manage them well the first thing you
want to know is what's the mode that we have the patient in are they in what's called CMV or controlled ventilation so this is a mechanical ventilation strategy where we actually set the respiratory rate that we want for the patient to have and we set the amount of tidal volume the volume that we want to deliver into the lungs this is usually good for a patient who is not taking spontaneous breaths and the other scenario if a patient is taking spontaneous breaths we should let them breathe on their own don't let them be dependent upon
the ventilator and so this is usually what we call PSV so it's called pressure support or patient control ventilation where you can actually allow for the patient to breathe at their own respiratory rate and their own tidal volume all you do is you set the peep in the F2 that leads to the next step often times in the exam they may say okay you have a patient who is being ventilated their pco2 is really High what do I do to reduce their pco2 well I want you to remember two things one is respiratory rate and
tital volume if you increase the respiratory rate or you increase the title volume it'll drop the pco2 if you have to pick between the two respiratory rate is going to be the more effective one same way test your knowledge if the pco2 is low what do you need to do then you need to decrease the respiratory rate or decrease the title volume because that will help to bring it up you're just trying to reduce their ventilation so pco2 is tied to respiratory rate and title volume the next one is pa2 what if it's too high
well if the pa2 is too high that may sound dumb but what do I want to do I don't I want their oxygen to be really high no it's actually kind of dangerous you want to reduce the peep or the F2 and that'll reduce the P2 same scenario P2 is low increase the peep or increase the F2 that'll increase the P2 the concept behind peep is that here's an alvioli it's not getting good ventilation you give them a lot of pressure at the end of expiration and they don't collapse they stay stented open and big
so now they can perform good ventilation and they can actually perform gas exchange but if you take the peep away they'll D recruit go back to that small size and they won't perform good ventilation so this keeps the alvioli stented open and it'll be able to perform gas exchange that's one of the big things about peep what about Pip this is called positive inspiratory pressure or Peak inspiratory pressure if the Pips are really high that means that there's a lot of resistance to air flow through the ventilator tube maybe it's a small tube maybe it's
kinked Maybe there's a lot of mucus within the tubing or they're having intense Broncos spasm that's important to remember if the Pips are low that means that there's probably something wrong with the ventilator circuit there's probably an air leak somewhere the big one here that I really want you to remember is called the plateau pressures Plateau pressures are a measure of kind of the uh if you take an inspiratory hold it kind of gives you the pressure within the airway at the at the end of inspiration so it's really important for helping to determine the
risk of lung injury if Plateau pressures are really high that means that the lung compliance is not very good a patient likely has ARS or pneumonia or things to that effect or they're air trapping a lot and so this is really dangerous and so whenever patients have very very high Plateau pressures it's important to reduce the tidal volume so you don't cause Barrow trauma to the lungs the last thing I want to talk about is whenever you have a patient who maybe is was intubated for a particular issue and you improve that underlying issue you
don't want them to be on a ventilator forever so you want to get them liberated from it and so what we do is we do what called spts or spontaneous breathing Tru and we look at a couple different thing did they resolve the reason why they were intubated and if they did good that's one thing second thing is is their F2 requirements very very minimal okay good is their peep really really minimal good is their risbey which is their rapid shallow breathing index are they breathing really really fast and not taking very good deep breaths
these are all things that would say that a patient would likely succeed and be able to be excavated if they don't meet these criteria you should probably not activate them because they'll have a high risk of being reintubated big things that I really want you to remember is V ventilating a patient comes with complications if you have really high title volumes in these patients especially in ards or really high Plateau pressures you can really rupture those alvioli and cause bar trauma that's one really big thing it can cause what's called ventilator induced lung injury you
want to avoid that the other thing is that you don't want to give them too much oxygen because if you give them too much oxygen you cause VQ mismatching you cause a lot of free radical formation a lot of inflammation that can also worsen the actual lung disease so avoid that and lastly is that these patients are high risk the longer they remain intubated the longer there is the risk for them to develop a VAP a ventilator Associated pneumonia so you want to try to liberate them as soon as you can from that all right
my friends that covers a monster of a topic in that being respiratory failure I hope it made sense I hope that you guys enjoyed it and as always until next time [Music]
Related Videos
23:45
Venous Thromboembolism (DVT, PE) | Clinica...
Ninja Nerd
69,646 views

46:22
Chronic Obstructive Pulmonary Disease (COP...
Ninja Nerd
163,646 views

20:25
Respiratory Failure EXPLAINED!
ICU Advantage
208,631 views

16:20
Respiratory Therapy - Type 1 vs Type 2 Res...
Respiratory Coach
29,212 views

53:42
Pleural Diseases: Pleural Effusion, Pneumo...
Ninja Nerd
64,953 views

19:54
Types of Shock (Cardiogenic, Hypovolemic, ...
Dirty Medicine
404,713 views
28:57
Pulmonary Sleep Disorders: Sleep Apnea, Ob...
Ninja Nerd
18,976 views

34:43
Asthma | Clinical Medicine
Ninja Nerd
187,954 views
38:06
Acute Respiratory Distress Syndrome (ARDS)...
Ninja Nerd
75,664 views
36:19
Urinary Incontinence | Clinical Medicine
Ninja Nerd
39,593 views

20:13
Pulmonary Artery Hypertension | Clinical M...
Ninja Nerd
51,857 views
14:19
Acute Respiratory Failure
The ICU Curriculum
73,505 views

43:26
Bowel Obstruction | Clinical Medicine
Ninja Nerd
49,883 views
10:08
Emphysema (chronic obstructive pulmonary d...
Osmosis from Elsevier
1,092,905 views
43:06
Peripheral Arterial Disease | Clinical Med...
Ninja Nerd
30,216 views

40:29
Shock | Clinical Medicine
Ninja Nerd
64,693 views

29:57
Asthma Treatment, Symptoms, Pathophysiolog...
RegisteredNurseRN
1,294,666 views

35:33
Acute Liver Failure | Clinical Medicine
Ninja Nerd
52,936 views

34:56
Lung Cancer - Bronchogenic Carcinoma - The...
Medicosis Perfectionalis
238,167 views
27:52
Bronchiectasis | Clinical Medicine
Ninja Nerd
69,453 views