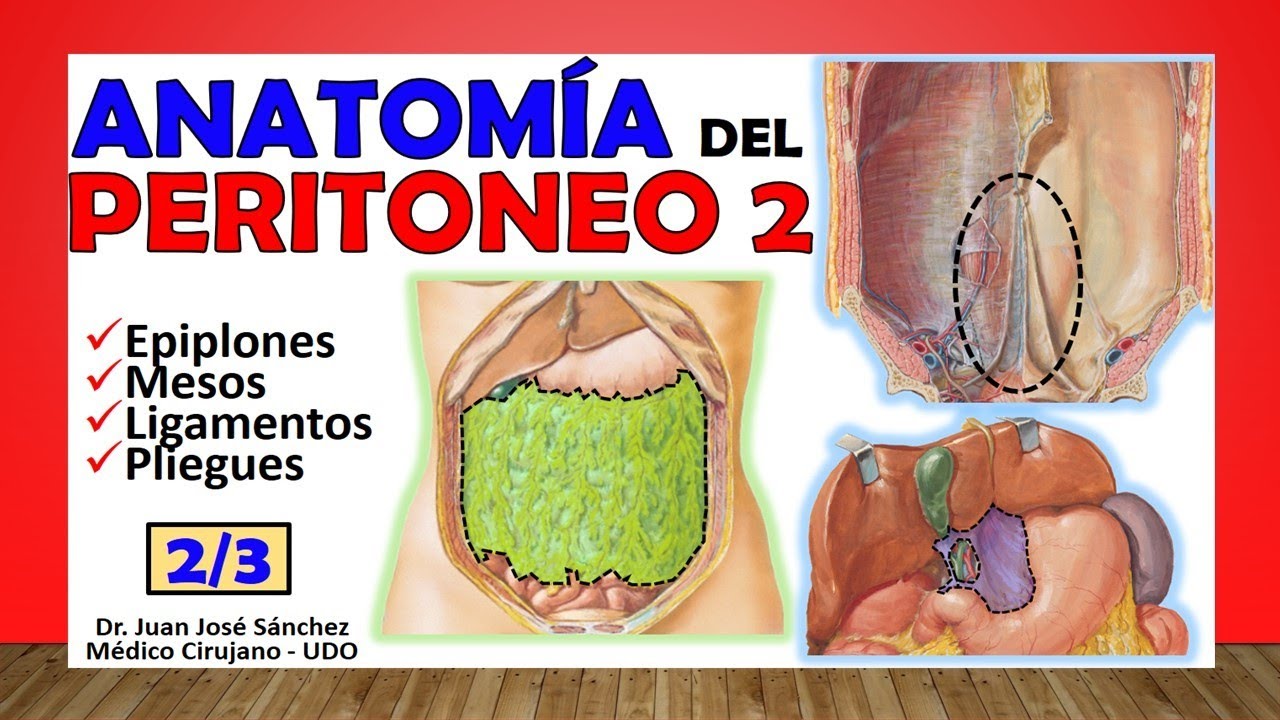
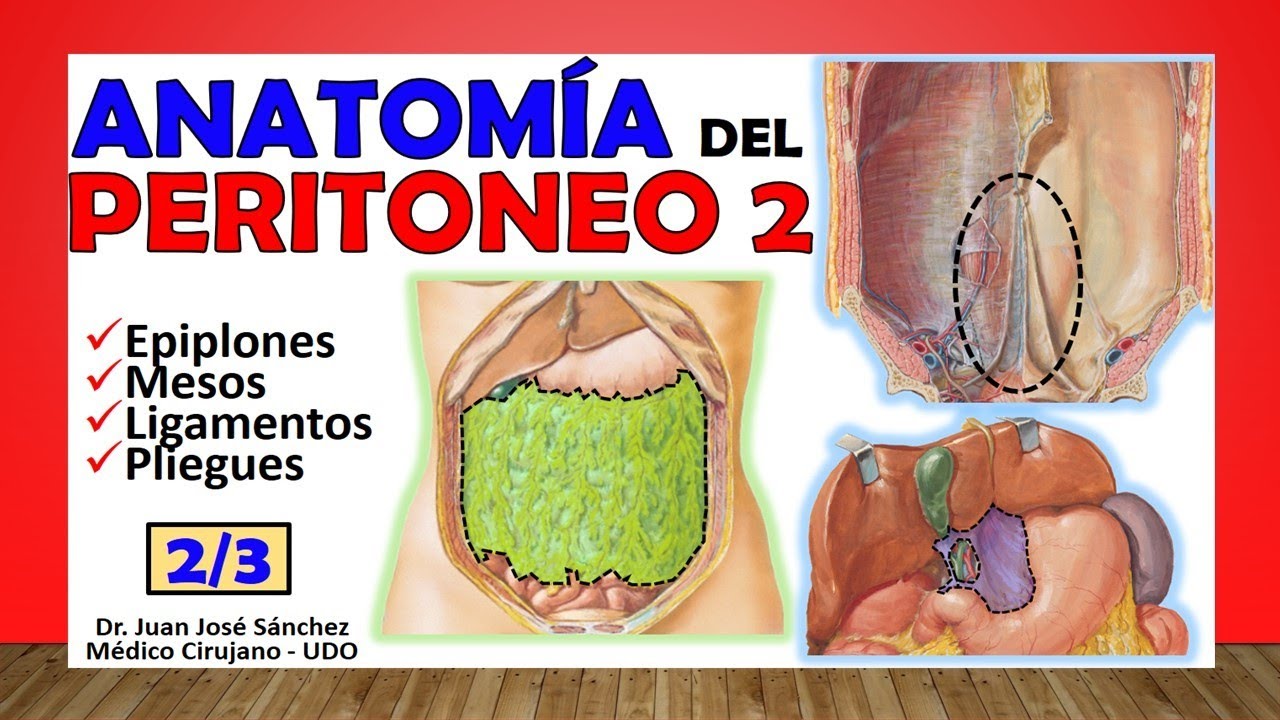
Hello how are you? Today we are going to see the second installment of this anatomy of the peritoneum, remember that I brought you three videos about the peritoneum and a fourth where we will talk about retro peritoneum, it is important that you see them in this order, that you see peritoneum one, two, three , then retro peritoneum so that you can fully understand this very complicated topic for students. So today we will finish talking about the great abdominal cavity and the strange, strange structures that you find inside it, we will talk about the omentums, we will talk about the mesos, the ligaments and folds, what difference does each of these structures have?
, then the Peritoneal folds are all those structures that are folds, it has no other name, it is like an extension of the parietal peritoneum that can become visceral when it forms these folds, generally these folds are to grab structures and fix them to the structures of the abdomen, they cannot be free even though they generally have structures that support them and keep them in a specific place, then there are three types of peritoneal replicas: they can be ligaments, they can be mesos or they can be omentums, the omentums also called oments, when we go What to name the ligaments? well, the fold is going to be called a ligament when we see structures that can join organs to each other, they can join organs in the abdominal wall but do not have important vascular structures, they are simply support structures, other times we call a fold or ligament when they are simply elevations of the peritoneum that do not have a supporting function but are simply that when the parietal peritoneum is superimposed on some structures it makes elevations and these elevations are called folds or ligaments without having any support function as such, then there are many ligaments within of the abdomen, imagine countless, each one of them I wrote in the corresponding part and in the easiest way for you to study it, that when you study, for example, the stomach, you study which are the peritoneal folds that support the stomach, when you study the Liver study the peritonial folds that support the liver, as well as the vessel and the duodenum, so and so on. Today we are going to talk about some ligaments that I have not named, which are the ones that are mentioned the most in the books within this part of peritonial folds that the posterior face of the anterior wall of the abdomen has, we are going to find a total of 6 folds in This level, this level here, this level is the navel and of those 6 folds, only one is above the navel and the other five are below , the one found above the navel is called the falciform ligament of the liver, Sickle-shaped means sickle-shaped, okay?
then this falciform ligament of the liver, see there that it is the parietal peritoneum that we try to fold looking towards the navel and forms two leaves: a leaf that I know would be the right leaf and a leaf that would be the left of the falciform ligament, so It is the one that joins the liver to the anterior abdominal wall and something important about it is that the inside contains on its free edge specifically the teres ligament of the liver, the famous round ligament of the liver, so do not confuse falciform ligaments with round ligaments, The falciform ligament contains the round ligament and that round ligament of the liver is nothing more than the obliterated umbilical vein. After the child was born, the umbilical vein became fibrous and formed that round ligament. If we see it here, this is an earlier view of the liver.
, this would become the right lobe and within the left lobe there we can easily see the two sides or the two leaves that form the falciform ligament, in the right leaf and the left leaf right in the middle of the liver, well it is worth telling you the place that separates the right anatomical lobe from the atomic union at its free edge, here you would find the round ligament that goes towards the liver, here so that you can more or less understand this cut, this little piece here is the falciform ligament, see how it holds or joins the liver to the anterior abdominal wall in this cross section that we have used a lot and we will continue to use it because it describes certain characteristics of the peritoneum very well, so we already know which is the only one of those six ligaments that is above the navel; let's now look at the five that are below the navel and we start with the only one that is odd of them of the lower ones which is the middle umbilical ligament also called umbilical fold, notice, this middle umbilical fold is when the parietal peritoneum is placed on top of this fibrous duct called urachus, that urachus is an embryonic duct that connected the bladder with the navel, literally with the navel, so when the child is born it no longer needs that, it becomes fibrous and that is the famous urachus, when that urachus becomes fibrous it is lined by the parietal peritoneum and becomes the middle umbilical ligament almost interchangeably called middle umbilical fold , we would carry two then, then we find the internal umbilical ligaments that are two to carry four or internal umbilical folds, also as the internal in anatomy is called medial, some books call it medial umbilical fold or ligaments, how is that fold formed ? medial umbilical? Well, that is when the peritoneum, as you can see here, rests above the obliterated umbilical artery, then the umbilical artery becomes fibrous, practically transforms into an umbilical ligament, and when the peritoneum passes over it it transforms into an internal umbilical ligament or umbilical fold.
internal, we would take four because it is one on each side, plus the middle, plus the falciform and then the other two that are below the navel are going to be the external umbilical ligaments, lateral umbilical ligaments or external umbilical folds, they are going to go more or less from the deep inguinal ring, which is this, to the level of the arch of Douglas, in these external umbilical ligaments, it is when the parietal peritoneum rests above the inferior epigastric vessels, which is the inferior epigastric artery and the inferior epigastric vein. Very well, we already know then what those six real ligaments or folds related to the anterior abdominal wall are, now, what complicates this issue is that pits are formed between these ligaments, we would then have between the middle umbilical ligament and the medial one, which is the internally the internal inguinal fossae, this internal inguinal fossa is also called the medial inguinal fossae and how it is above, see how it is above the bladder and above the pubis they are also called the supra-vesical fossae, the supra-vesical fossae because they are above the bladder; then we go to one side and this would be in some fossae that are between the internal umbilical ligament and the external umbilical ligament, this would be the middle inguinal fossae, also one on each side, something important is that in this middle inguinal fossa there is this triangle We are going to know what it is right now, then we would have the fossae that are lateral to the lateral or external umbilical ligament, which would be the external inguinal fossae or lateral inguinal fossae, these are the fossae in relation to the ligaments, this triangle that is found here in The middle inguinal fossa is the famous inguinal triangle or Hesselbach's triangle, a triangle that we name the limits when we talk about the inguinal canal, I want to make a video just about Hesselbach's triangle, even though it is easy, it is very important between the point From the study of hernial pathology of the abdomen, what I want you to know about this Hesselbach inguinal triangle is that it is located within this middle inguinal fossa. Very well, you already know what a ligament is, so let's now talk about what an omentum or omentum is, when I can call it an omentum or omentum, what are more or less the characteristics of these omentums, but first don't leave the video [Music] I invite you to subscribe here in the lower right corner click [Music] and don't forget to like the video.
It is important that you subscribe to the channel where I clicked, again you would apply and you would automatically be subscribed to the channel and access all the anatomical content, more than 160 videos of all anatomy and some that I still have to do that I am not even going to half of what I plan to do. These omentations u Oments are structures of visceral peritoneum that join, listen well, they no longer join wall with viscera, this joins viscera with viscera and therefore important vascular pedicles generally run through them, that is, there are arteries and veins that run between these structures. We are going to talk generally we know two large omentum, the most current name is omentum, sorry the most current name is omentum, which is the greater omentum and then we will talk about the lesser omentum.
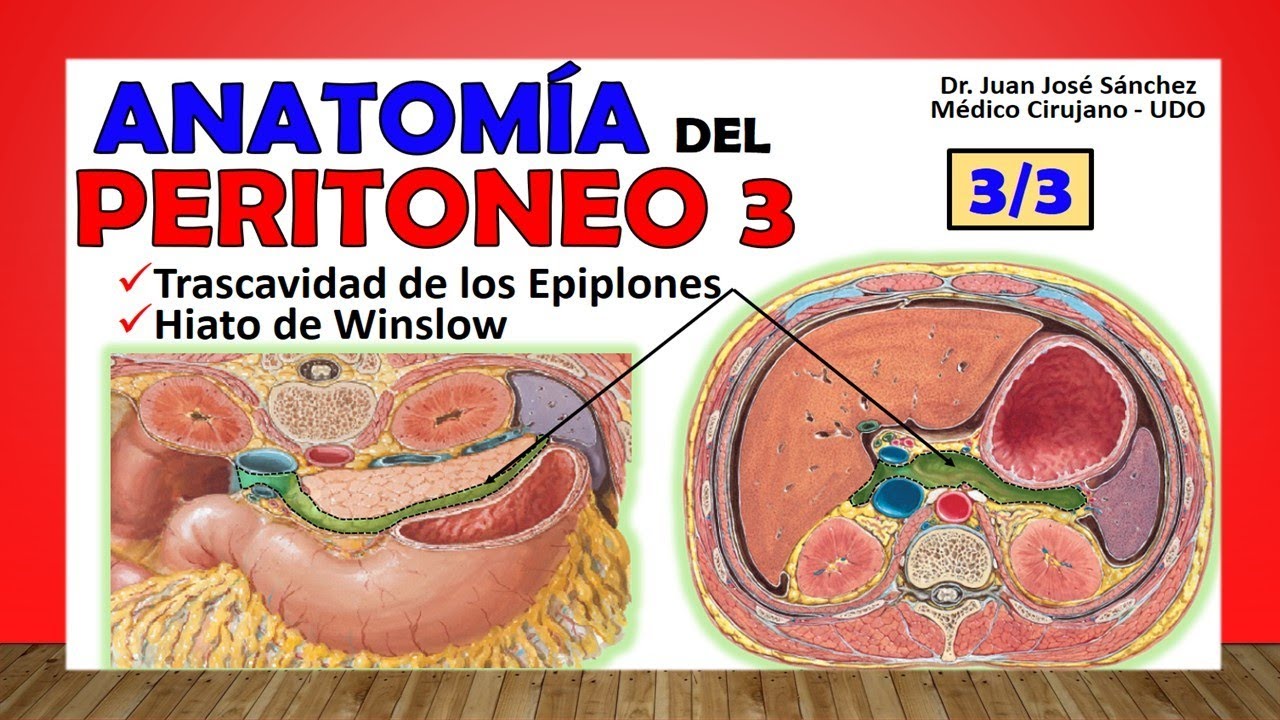
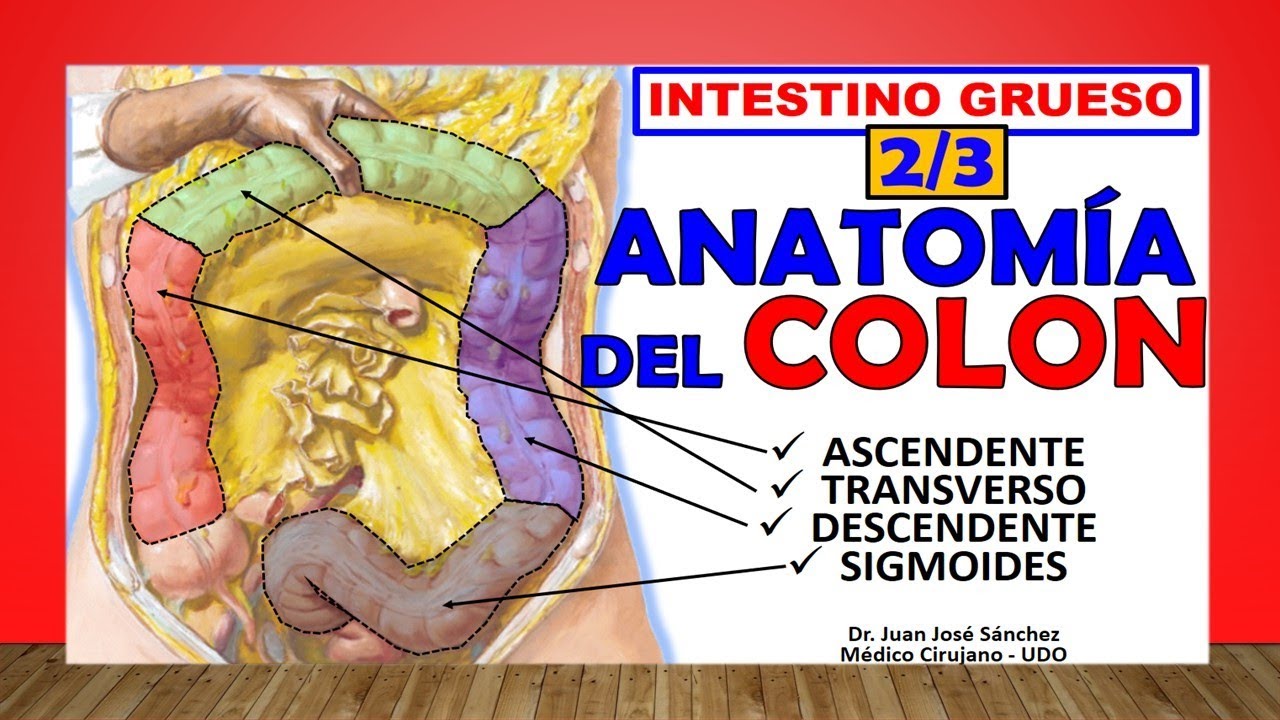
Let's start talking about this greater omentum, which is said to hang literally like an apron along the greater curvature of the stomach, then heading downwards. It is made up of four leaves, although some books say two but there are really four, since I explain why and this is going to have insertions at the level of the transverse colon, the descending colon and the ascending colon, in fact when you see here we separate them from the ascending and descending colon and let these structures that are the epiploic appendages, that is the famous greater omentum, practically the entire inframesocolic compartment, is like an apron, that greater omentum is literally like an apron, here you can see how it originates along the entire greater curvature of the stomach and it can also be seen It has insertions at the level of the transverse colon, so you will say: how is that thing that is made up of two leaves or is it made up of four leaves? well, they describe two leaves, an anterior leaf and a posterior leaf, an anterior leaf that is the one that reaches the entire greater curvature of the stomach and a posterior leaf that is the one that has direct insertion into the transverse colon, however these leaves each one is made up of two sheets, let's say that the anterior sheet has an anterior sheet and a posterior sheet, the posterior sheet has an anterior sheet and a posterior sheet, there is a space that remains between the two middle sheets and that space that remains is the lower part of the transcavity of the omentum, however the majority of this space, here they were put in blue so that they understood that a space existed, but the majority of this space is closed, when the child is born it is already closed and Practically only the upper part is the only one that remains open, this omentum derives from the dorsal mesogastric, it is important that you know that from an embryological point of view, then you already know how the leaves of the greater omentum are arranged; So now we talk about the lesser omentum, that's why the greater omentum runs in an artery that is the gastroepiploic or gastro-omental artery , both the right and the left, leaving that as one, the entire vascular pedicle that goes towards the greater curvature of the stomach, passes through the root of that greater omentum, in the lesser omentum see how it follows with the omentum theory, that is, an organ with an organ, this lesser omentum is an omentum that is composed of two ligaments, one that is wider and is more towards the left, would join the liver with the lesser curvature of the stomach that would be the gastrohepatic ligament, it is said that in the gastric root of this gastrohepatic ligament that starts from the lesser omentum in this root is that the left gastric artery runs with the right, the coronary stoma with the pyloric artery, it anastomoses and makes an arch at this level, then we have one that is a little thicker but smaller that would join the liver with the first portion of the duodenum is the hepatoduodenal ligament, then the lesser omentum It would be made up of the gastrohepatic ligament and the hepatoduodenal ligament.
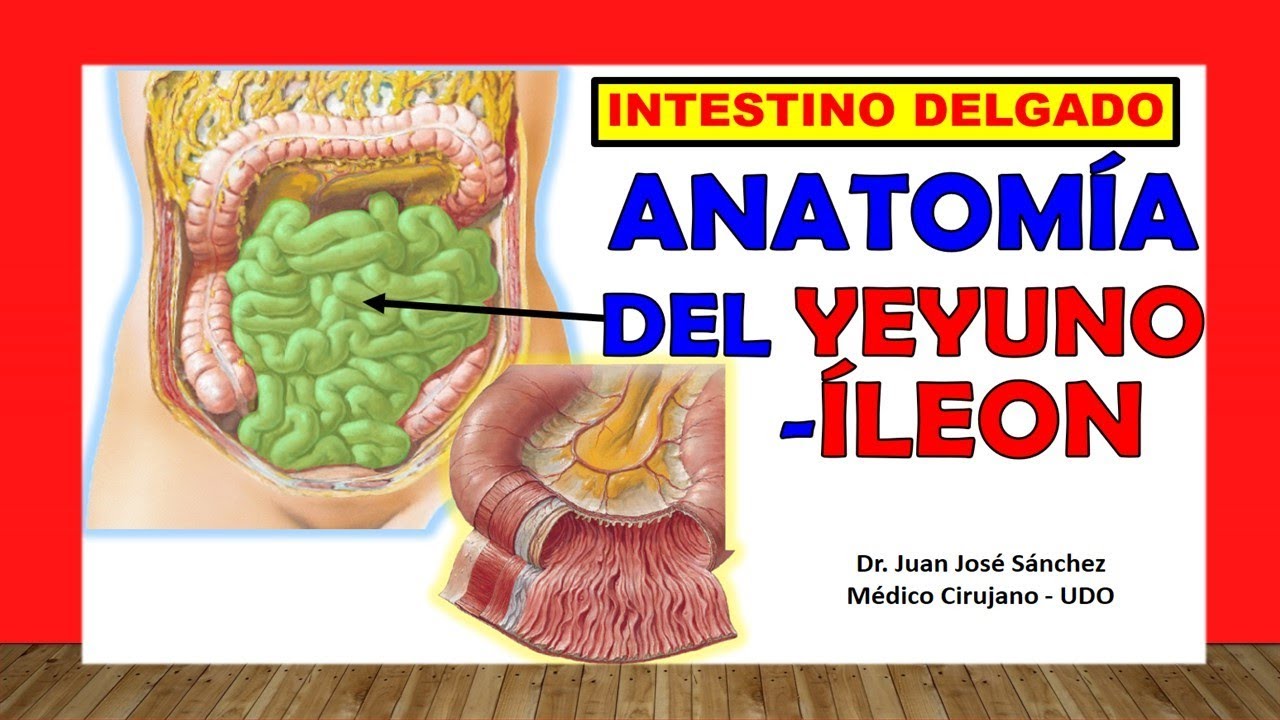
This hepatoduodenal ligament is very important because when we cut it we can find the famous portal triad, the famous hepatic pedicle, the famous Gleasson's pedicle is inside that hepatoduodenal ligament, What is the common bile duct with the proper hepatic artery and the portal vein at the back, imagine, it is also said that it is going to form the anterior limit and on one of the edges of the entrance to the cavity of the omentums and that entrance receives the name of winslow hiatus, I remind you that in the third installment of peritoneum we will address that famous recess of the omentum, finally we will talk about the ligaments and we will talk about when it is an omentum or omentum; now let's talk about when in a meso, what a meso? A meso is a structure that joins the posterior abdominal wall with an organ but it is vascular, vascular as well as an omentum, that is, it has important vascular structures which separate them from the ligaments, these mesos are going to support the omentum in parts of the tube. digestive, let's first find the mesentery, which is responsible for joining the posterior abdominal wall with most of the small intestine, see how the entire inframesocolic compartment passes through it, it is said that the root is 15 centimeters long, that is from here it begins to grip the jejunum in the duodenum-jejunal angle until the ileum practically empties into the cecum and there measures 15 centimeters, it is the root, it is the origin of that mesentery, the visceral edge will be the edge that joins the intestine , that is, from the jejunum to the ileum, because the duodenum does not need the mesentery, this visceral edge measures what the intestine measures, this intestine measures 5 to 6 even up to 7 meters from the portion of the small intestine and that is what It will measure the free edge, in fact that is why it is wrinkled with that fan shape; Now wide, what is the width?
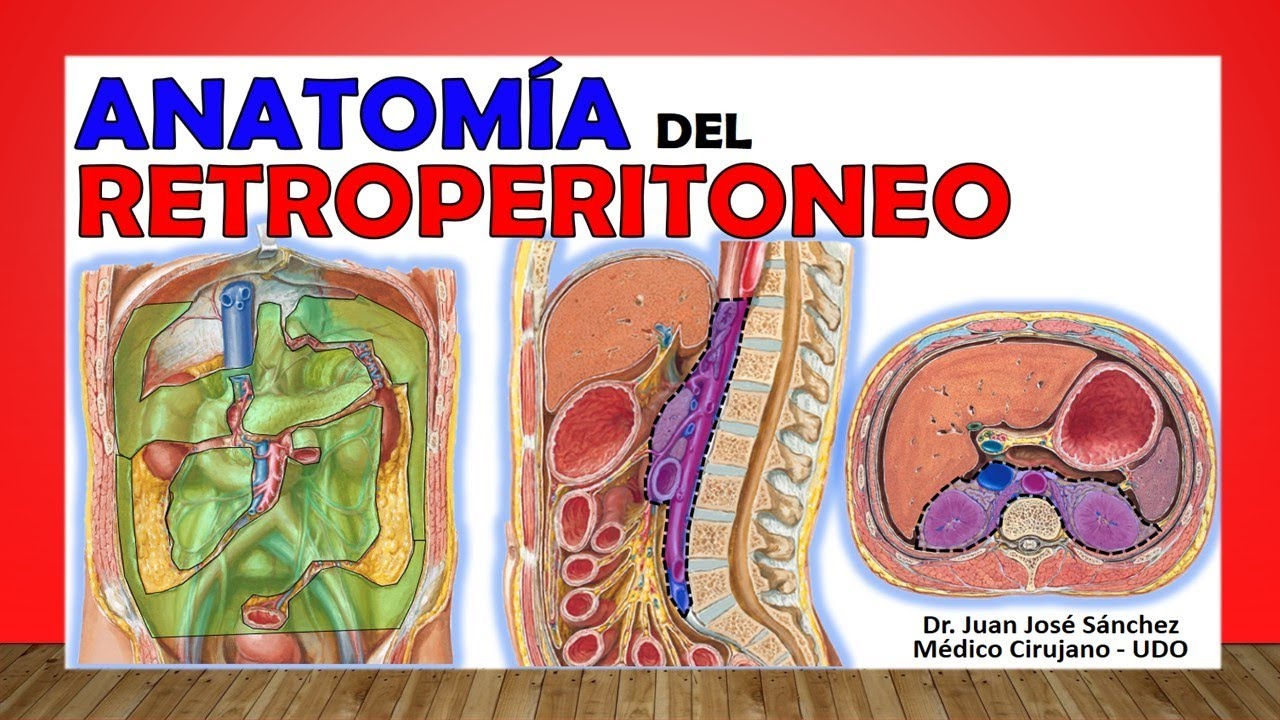
width of what goes from the root to the visceral edge, that width can measure up to 20 centimeters wide, in my video of the duodenum and jejunum I address the characteristics of this mesentery much more deeply, remember that here we are seeing it in one Generally speaking, this mesentery, which will also be made up of two leaves, is the one that contains the mesenteric vessels superior to the superior mesenteric artery and vein, which are the structures that drain and irrigate the jejunum and the ileum. They run within that mesentery, now the root is going to go from here, the duodenal-jejunal angle to here, the duodenal-jejunal angle coincides with the L1 vertebra and it is said that the iliocecal junction is the final part of that mesentery because the ileum is supposed to end there. , that is more or less at the level of the right sacroiliac joint, here we can see the two leaves that make up the mesentery and since there would be the superior mesenteric artery and the superior mesenteric lamina, here we can see how it grabs the loops of the intestine thin, the transverse mesocolon, well important because the colic arteries, part of the right colic artery and part of the left colic artery, reach the transverse colon thanks to it, this transverse mesocolon is the one that would support the transverse colon and make it hang there in its particular position, see there that transverse mesocolon, it would also be formed by two leaves, an upper leaf, see how it is attached to the parietal peritoneum that covers the pancreas and a lower leaf that is attached to the parietal peritoneum that covers the duodenum, the third portion of the duodenum specifically and what it had in the middle is the transverse mesocolon itself, here we see the vascular pedicle of the middle colic artery is specifically, here we would see the transverse colon, here we can see the root of the transverse mesocolon that it crosses both kidneys, kidney left and right, to the second portion of the duodenum, to the pancreas in its entirety, the head, the body, including the tail, this is the famous root of the mesocolon, that is where it is holding on, the ascending mesocolon It is important to study it because it does not always exist, in fact most of the time there is no ascending mesocolon and in those cases where there is no ascending mesocolon it is said that the descending colon would become a retroperitoneal structure, do not miss it, look for the retroperitoneum video so that you understand why I say that this retroperitoneal, while there is never a descending mesocolon, the descending colon will always be part of the retroperitoneum specifically, the mesoappendix, see, is a structure that is also a peritonial fold that supports the appendix, important because the appendiceal artery runs on it to be able to reach the appendix, here we can see how there is nothing that supports the descending or ascending colon, the same parietal peritoneum simply folds in front of it but does not make it hang, there is no vascular pedicle, it is important therefore this would practically be retroperitoneal viscera, the only caveat is that the ascending mesocolon exists, in which case the ascending colon is not retroperitoneal only and only in that case.
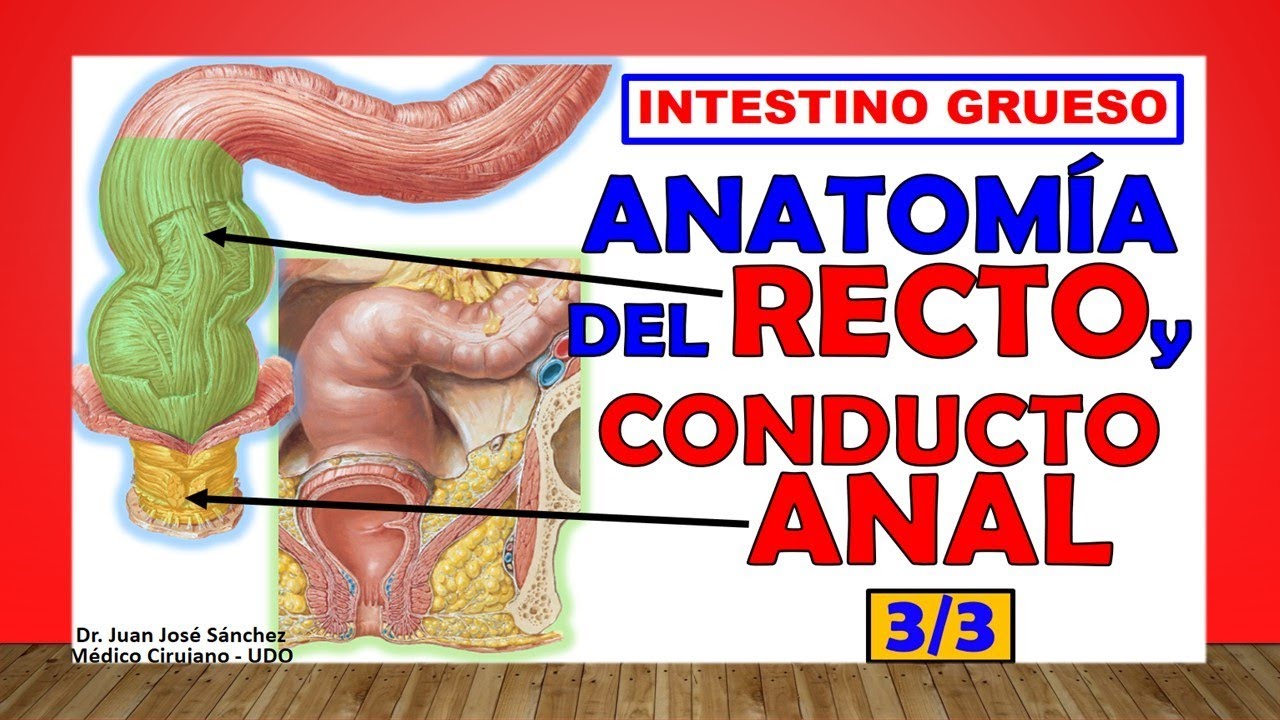
Finally, the sigmoid mensocolon is a structure that supports the sigmoid colon in its entirety and joins it to the posterior abdominal wall. Likewise, the sigmoid arteries, which are branches of the inferior mesenteric arteries, reach the sigmoid colon through the sigmoid mesocolon. Here we can see the entire root of that sigmoid mesocolon and this is when it becomes specifically straight.