foreign what's up Ninja nerds in this video today we're going to be talking about heart sounds and heart murmurs again this is going to be part of our clinical medicine section if you guys like this video it helps you please support us one of the ways that you can do that is by hitting that like button commenting down the comment section and also subscribing another thing down in the description box below we have a link to our website on there you'll find a lot of great stuff we got notes we have illustrations we're developing exam
prep courses for those of you taking the step one the step two the pans Etc and we have some nerd and engineer merchandise that I you know think you guys should check out as well all right without further Ado let's start talking about heart sounds and heart murmurs when we talk about these I think it's really important for your exams and also for the clinical world to be able to understand normal heart sounds when there's some extra heart sounds like S3 and S4 and if you really want to go to the advanced level if you're
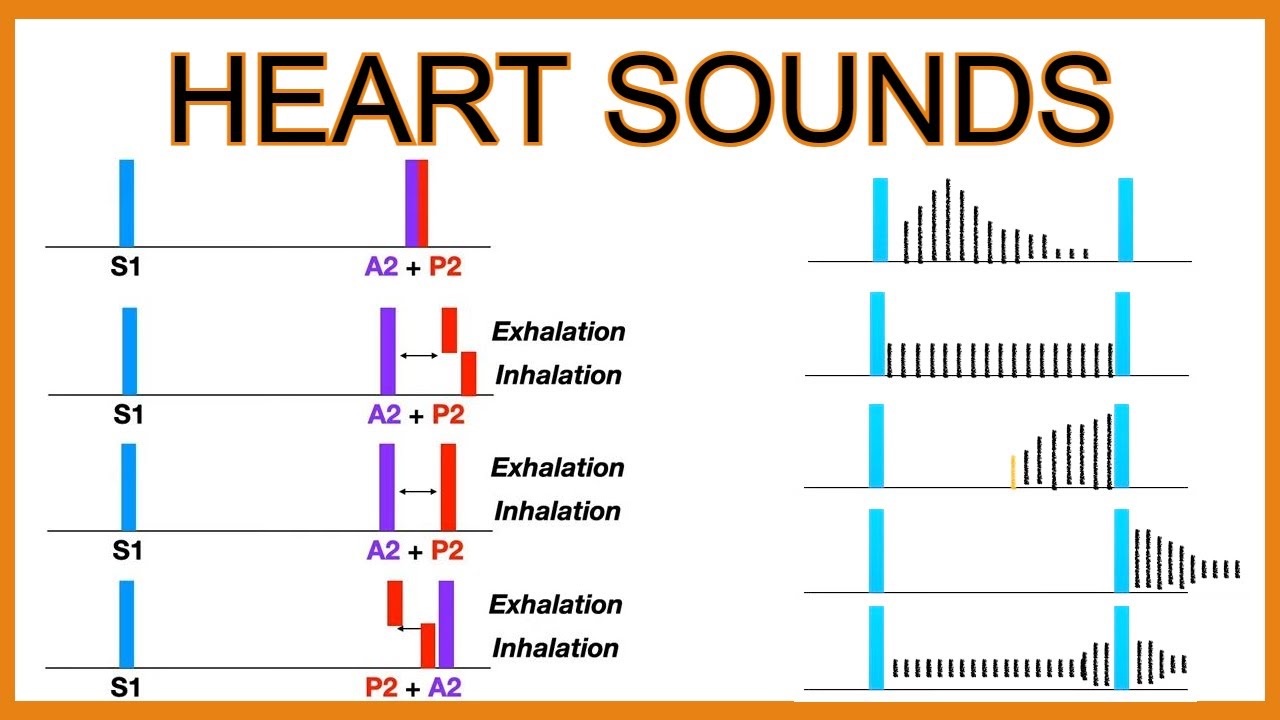
planning to go into Cardiology then I could say let's talk about the splitting of the S2 all right so first things first real basic stuff here S1 S2 heart sounds these are the normal heart sounds so S1 which you're going to represent on this graph with the time on the x-axis is going to be this guy here this is our S1 S1 is going to represent two things one is it's going to represent the closure of one of the valves which is going to be the mitral valve so the mitral valve should close because what
happens is as the pressure inside the ventricles rise and it tries to push blood out of the left ventricle into the aorta it should close the mitral valve same concept as blood is going from the right ventricle into the pulmonary artery it should open the pulmonary valves but close the tricuspid valves so for S1 it should be the closure of the mitral valve and the tricuspid valve should close and then subsequently the aortic valve and the pulmonary valve should open that's the basic concept behind that but the sound is the closure of these valves S2
is the opposite so blood is already exited the left ventricle in the right ventricle it fills the pulmonary artery and fills the aorta what happens is during diastole some of the blood will try to recoil we don't want it to go back into the left ventricle so we should close the aortic valve same concept blood from the pulmonary artery will want to kind of fall back into the right ventricle but it shouldn't be able to go back into the right ventricle because of the pulmonary valve should snap shut so whenever these two valves snap shut
that is the S2 heart sound so it'd be the aortic we're going to put a little o there aortic valve closing and the pulmonary valve will also close one important thing to remember though is that the aortic side it's the pressure is really kind of high and so naturally the the actual aortic valve should close quicker than the actual pulmonary valve should so sometimes we represent this S2 as two parts we represent an A2 which is the second heart sound which is the closure of the aortic valve and pulmonary valve but particularly the aortic component
and then the other component here is the P2 which is the pulmonary valve closing which is a component of the S2 but both of these make up the S2 okay all right that's the basics what we're going to do is we're going to add in some sounds and talk about the splitting of the aortic and the pulmonary vowel sounds for the S2 let's come to the S3 and S4 so S3 and S4 are interesting sounds they're extra heart sounds so now we should know that you'll have an S1 and then you'll have this A2 and
P2 so we're going to put S1 and we're going to put A2 and P2 that's the S2 hearts on though you add another heart sound in this which we're going to talk about is S3 S3 the concept behind this is there's left ventricular dilation that's the words I want you to remember there's left ventricular dilation so these ventricles are gargantuous and so what happens is the actual left ventricle can easily fill they actually rapidly fill with blood and as they rapidly fill the blood bounces off the walls of the ventricles as it starts to distend
and it creates this turbulence of blood flow which triggers a murmur that is that turbulence of blood flow within the super dilated rapidly filled ventricles is the S3 heart sound so again just to recap it it's going to be rapid ventricular we're going to put in this case left ventricular filling which creates a massive turbulence of blood flow within the left ventricle and you could say the right ventricle and that is what precipitates the actual extra heart sound all right so that is going to be the S3 so this will precipitate what sound the S3
so then we have to ask ourselves the question what's the reason for the rapid left ventricular filling super dilated ventricles what are some causes of dilated ventricles CHF which one systolic heart failure so one cause would be systolic heart failure the other one would be dilated cardiomyopathy would be another really really big one this can happen not just pathologically but physiologically sometimes in patients who are super young and healthy athletes they can have dilated ventricles so they can trigger super large stroke volumes so you can't see this as well in young athletes so these are
the concepts that I want you guys to understand is the causes whether it be pathological or physiological of the S3 so we know that it's during the filling process so that means that these valves are open the mitral valve and the tricuspid valve are open so if those are open it can't be after the S1 it's got to be after the S2 because they're closed from S1 all the way to S2 during S2 after that they open up a little bit again so the sound would have to be right here and have to be very
early so what we're going to do is we're going to add in this extra sound here we'll do it here where there's going to be a sound that comes right after this and this is going to be the S3 so you'd have S1 the S2 which is the combination of these and then right afterwards the S3 if you have systolic heart failure cardiomyopathy are very young healthy athletes let's go into this next one so S4 heart sound what do you notice the difference between the ventricles here thin super dilated ventricles thick ventricles so whenever you
have a very rigid left ventricle it actually will do what it will decrease ventricular filling and if you decrease the ventricular filling process what this does is this causes the Atria to have to generate a very high pressure and so the Atria will contract super late so you develop a late atrial contraction because the Atria are going to have to really really work very hard to push blood from the Atria and the ventricles because of the super high pressure of the ventricles and how poor their filling process is so again rigid left ventricle will decrease
the ventricular filling that'll make it really hard to get blood into The ventricle so then the Atria has to contract and very powerfully and when it does it generates the S4 heart sound so the S4 heart sound is usually the result of the atreus super working hard to contract and squeeze blood down so it goes hard to get blood in whenever that happens and it makes it difficult to get blood in the Atria will then pound on the remaining blood in the Atria to squeeze it down into the left ventricle that is referred to as
the S4 heart sound but it comes later so it has to go S1 A2 P2 which is your S2 and then in comparison to S3 S3 will come right afterwards if you have a dilator rapidly filled ventricle for S4 it has to come a lot later because now the H we have to contract to push the remaining amount down so this would be your S4 and S3 will be somewhere in here as comparing the two so now we've compared S3 and S4 the question comes is what's causing this rigid left ventricle to not fill diastolic
heart failure that would be a big one where they're super super kind of hypertrophic and very poor at being able to fill another one is anything that causes left ventricular hypertrophy what are two things that cause left ventricular diversity aortic stenosis this will definitely precipitate left ventricular hypertrophy and if you hypertrophy this Can you feel it no it's a very small space and the last one is chronic hypertension this will also precipitate left ventricular hypertrophy so these are the things that I want you guys to remember for the causes of an S4 heart sound okay
beautiful at this point we covered normal s1s2 we've covered what happens when you have a dilated rapidly filling turbulent left ventricle and what happens when you have a rigid left ventricle with poor ventricular filling and the atrium to contract to push the remaining blood down S3 S4 accordingly now if you're a cardiologist level you got like that insane uh stethoscope in the ears of an eagle I guess and you can really really pick up on some of these things sure we can talk about the splitting of the S2 the concept behind this is when you
have a patient who's let's say we're in two phases so one is we're going to say that the patient is particularly having an inspiration and actually let's do it like this let's say expiration first and inspiration later so expiration first inspiration later what happens is you have that S1 and then you have again the S2 which is the A2 and the P2 naturally in normal people it should go A2 and it should go P2 and they should be really hard to be able to differentiate one another on the expiration but let's say that the person
decides to take a deep breath in when they take a deep breath in what happens is you massively fill the right ventricle because your intrathoracic pressure drops and if you feel the right ventricle this thing is going to get over filled more than usual during expiration if it's overfilled it now has to push a larger volume of blood that it usually does out of the right ventricle into the pulmonary artery during systole and then during diastole come back and snap it shut if it has to deal with more blood than it usually has to what
do you think is going to happen to that sound is it going to come a little bit earlier later stay the same it's got to push it a lot more it's going to come later so what happens is is you have something called the S1 the A2 will stay there but the P2 will just extend out a little bit more and that'll only happen during inspiration why because of increased filling so because of increased right side venous return the heart is on the right is going to have to deal with more blood during inspiration than
it usually does during expiration and that's the concept behind this okay so physiological split S2 is a physiological thing so the cause is usually it's due to resperophasic changes is that special way of explaining that the S2 can split during inspiration as compared to expiration that's all it is okay cool now we move on to the next concept of a split S2 a wide split S2 so this one's weird and what happens with this one is the patient usually has again their S1 is the same no change there but what you'll notice is is that
their actual again aortic sound and Pulmonary sound appear again farther away during expiration but during inspiration they appear even farther so here that's really hard to differentiate in physiologically Split S2 but in a wide split S2 you can actually differentiate the A2 and P2 and both expiration and inspiration so now we have to ask ourselves the question why am I able to hear the splitting of the S2 in both expiration inspiration and compared to the physiological one and that's because the right ventricle is being overloaded constantly or it's having a hard time getting blood out
of the right heart in general so let me explain something let's say that a patient has something called let's say a right bundle branch block let's say that they have a pulmonary hypertension where their pulmonary artery pressures are super high and it's really hard in both of these scenarios if I have a right bundle branch block this right ventricle is not going to contract on time it's going to delay the time of contraction the other thing is if I have pulmonary artery hypertension it's going to be harder for the right ventricle to generate enough pressure
to push blood out into the pulmonary artery that's going to delay the time to get blood out if either delay the blood getting out of the right ventricle that'll cause the pulmonary sound to come later in general expiration but then make it worse take a deep breath in you take a deep breath in and now your right heart venous return is going to increase now you give the right heart that's already struggling to get blood out even more blood and it's going to make it even longer so that's the concept here is that you're actually
extending this during inspiration but it's still present during expiration what's the reason why behind this the reason why is is again you're increasing the right Venus return in a strained right heart and if you overload that right heart it's going to make it even harder to take a longer time to get blood out of the right ventricle that's the concept here so for a wide split S2 think about right heart diseases right bundle branch block pulmonary hypertension anything that is delaying the transit of blood out of the right ventricle all right fixed split has two
this one's actually super super cool and I only want you to remember one of these but what happens in this one is again you're going to notice S1 S1 is not changing but what you're going to notice here is watch this this is actually kind of cool there is a splitting of the S2 the A2 and P2 component during expiration but it is if I can do this perfect exactly the same length apart so now this one it went from there's a split to holy crap there's a split from here there's a split and the
split's the same all right no split to a split split to holy crap there's a big split and split split same what in the heck is causing the split to be the exact same during both expiration and both inspiration okay good question the primary cause is something called an atrial septal defect that is it there is other ones but this is going to be the one that you'll most likely see on your exam what happens is during expiration the pressure in the left heart is higher than the pressure in the right heart so what will
it do it'll shunt blood into the right heart filling it with a good amount of blood so you're going to fill this right heart with blood and if it's going to fill it's going to take a little bit of a longer time to be able to squeeze that blood out of the right heart into the pulmonary artery and eventually close the pulmonary valve in comparison to the aortic valve during inspiration what happens to the Venus return to the right heart it increases because you're pulling blood from the Supreme vena cava and the inferior vena cava
filling the right heart with blood giving it more blood to have to deal with a longer Transit time between the right ventricle to the pulmonary artery and eventually shutting the valve so what you'll notice is is that the right heart venous return is fixed that's the cool thing about this is that there is a right Venus return that is fixed during both inspiration and expiration and what I mean by that is is that in this patient they're having blood coming from the left atrium to the right atrium during expiration because left atrial pressures are higher
and that the blood coming from the superior vena cava inferior vena cava going into the right atrium is occurring because of inspiration dropping the interthoracic pressure but the Venus return to the right heart is constant during inspiration and expiration that's the cool concept here and it's because there's a hole allowing for the equalization of blood flow because of the ASD that's the cool concept let's come to the last one here which is a paradoxical split S2 so this one's really kind of a wonky one what happens here is again you have that S1 that's going
to be the constant thing that you'll notice out of all of these this is the same but here's what's really cool you have the P2 that comes first and then the A2 comes after and you're like wait a second I thought that it always was a2p2 yeah this is why it's weird it's wonky right and the same thing during inspiration you'll notice that the P2 is still coming before the A2 it's just it's just a little bit closer so what you'll notice is you'll notice a reverse kind of of the reversal of the roles of
these two right and you notice that it's wider during expiration and less wide during inspiration let's dive into this okay so the only reason that the P2 would come before is because the left ventricle was taking probably a super long time to get blood out of it that's what was the common theme out of all of these before the reason why the P2 is becoming later or whatever it may be is because it was taking a longer time for the right heart to get blood out so if the A2 is coming later it's because it's
taking a long time to get blood out that's the whole concept so there has to be a delay and left ventricular expulsion of blood and therefore if there's a delay in the left ventricular expulsion there'll be a delay in the closure of the aortic valve and pulmonary valve of blood so we have to ask ourselves the question okay what's causing this well one is we're having a hard time getting blood out of the left ventricle into the aorta this part is not occurring very well what was the problem in this one it was because the
left the right bundle branch was actually blocked but what if the left bundle branch is blocked wouldn't that cause a delay in the left ventricular depolarization and contraction yeah so a left bundle branch block would be one particular reason the other one was that if a patient had like chronic hypertension right so if they have pulmonary hypertension same thing anything that causes the afterload to be super super high so usually this would be things like aortic stenosis would be a really really big one so aortic stenosis is a really one important one to remember oh
um hypertrophic obstructive cardiomyopathy where the septum is so thick and chunky that it blocks the blood flow out of the left ventricle that would be another one that delays the blood flow and again you could definitely add in systemic hypertension as well so we could add in systemic hypertension that's also going to be this one as well so all of these could definitely lead to the left ventricle having a harder time to get blood out of it delaying the blood flow getting out and then subsequently delaying the closure of the aortic valve and that's why
it comes later question is is in all of these we notice that during inspiration it increased that space between the two why is it increased in expiration and decrease in Inspiration well let's kind of use logic here during the process of expiration more blood flow is coming to which side of the heart to the left heart so it'll get filled with more blood it's going to make it harder to be able to get blood out already now add more blood it's going to delay the actual process even more inspiration you're doing what to the heart
you're increasing right side venous return if you increase right side venous return now the right heart is going to have a little bit more of a struggle to get blood out of it because it's going to have to deal with more blood so that should cause the P2 to come a little bit closer to the A2 because now it has to deal with a larger volume of blood expiration left ventricles to do with more blood inspiration right ventricles to deal with more blood that's why it just gets a little bit shorter during inspiration super cool
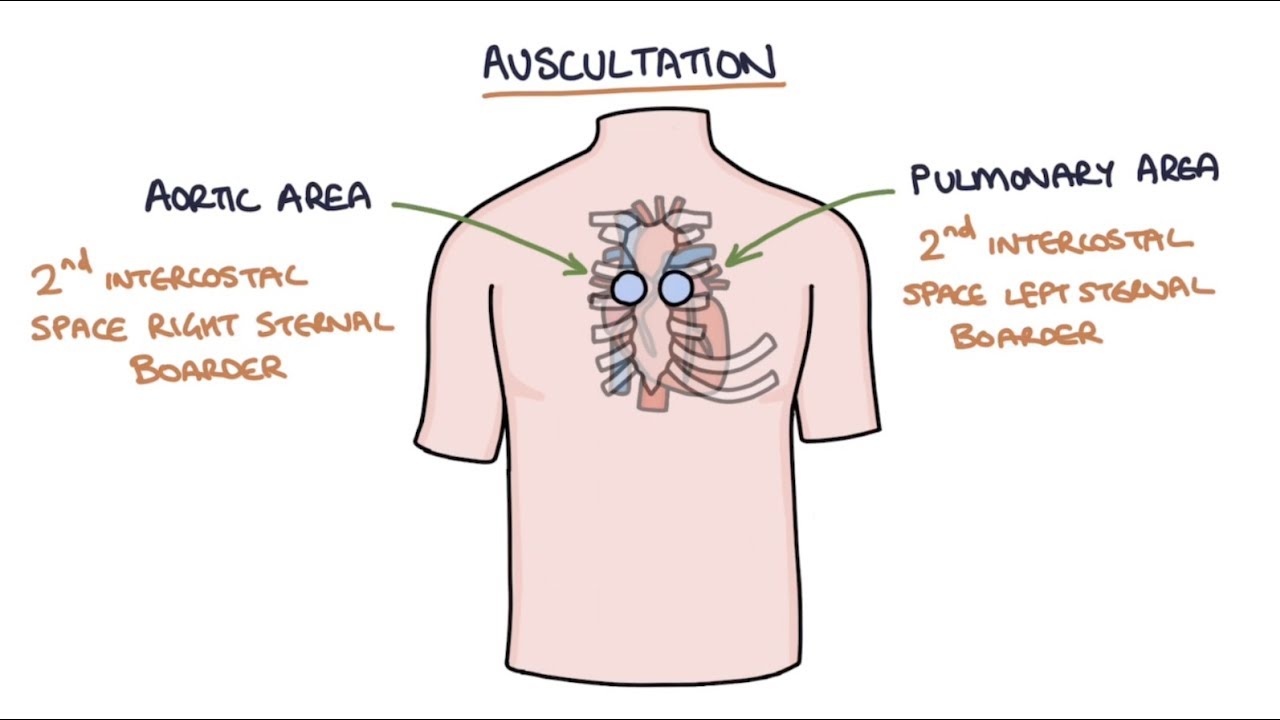
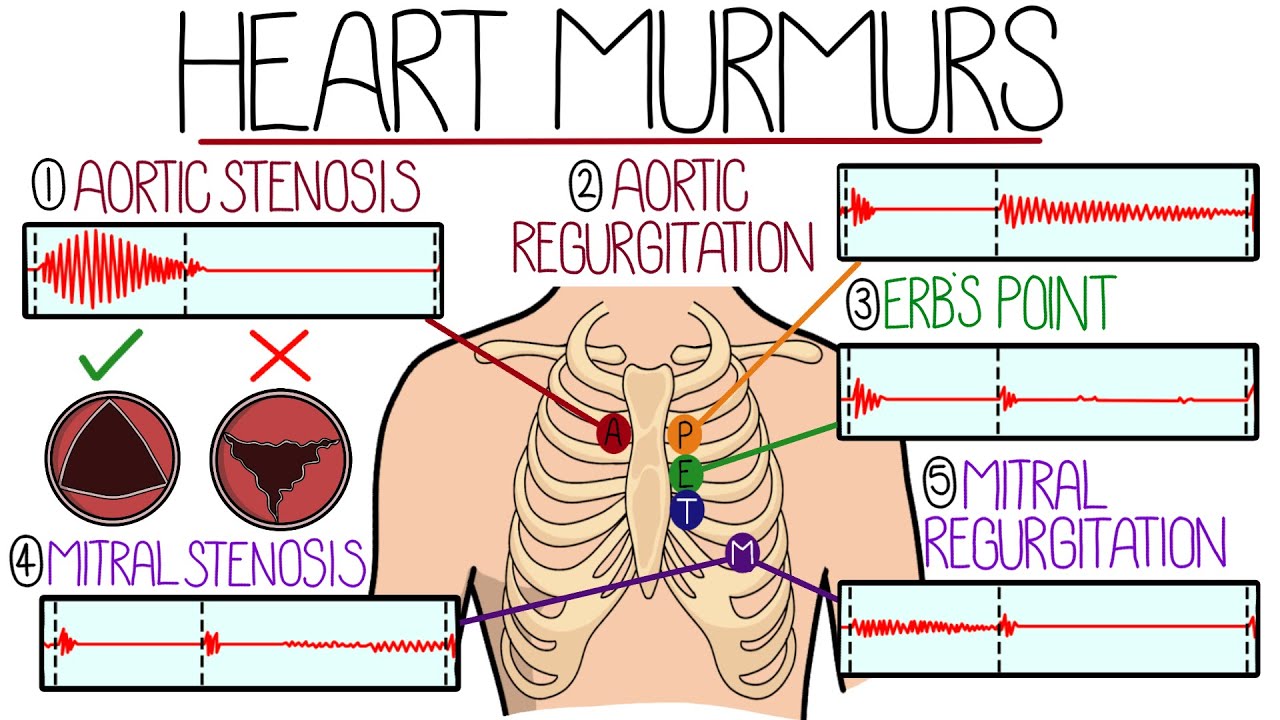
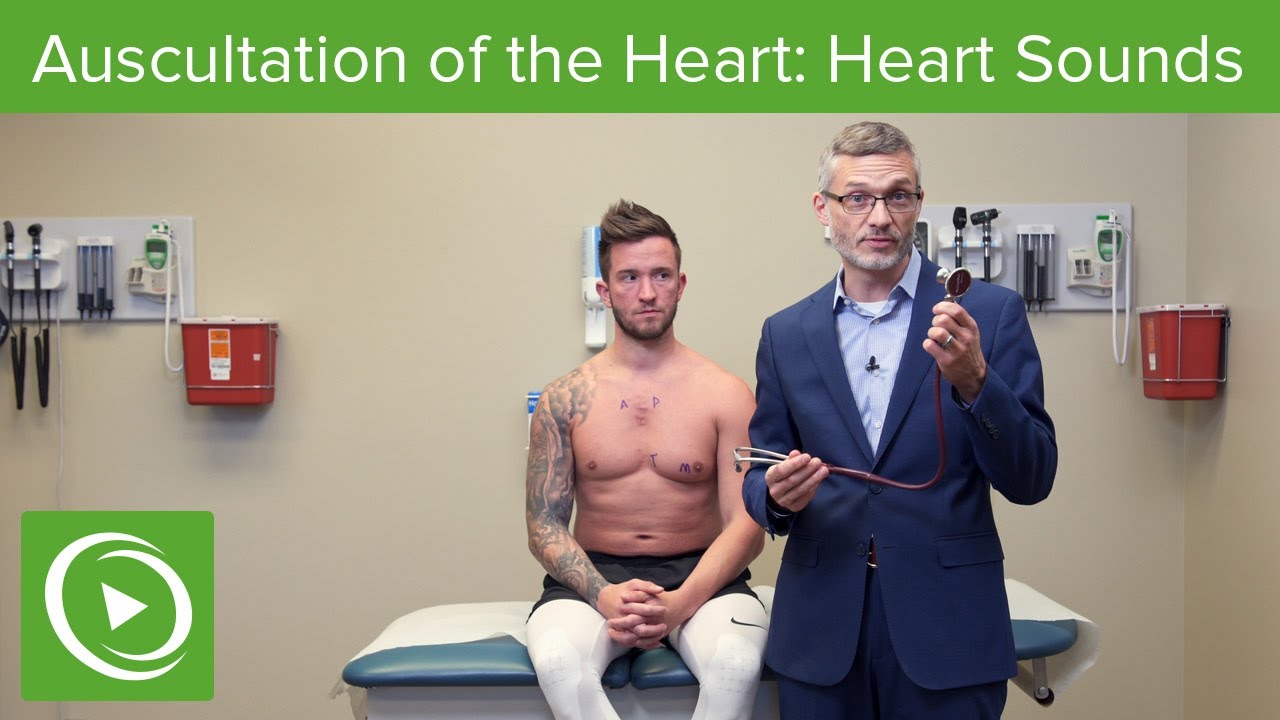
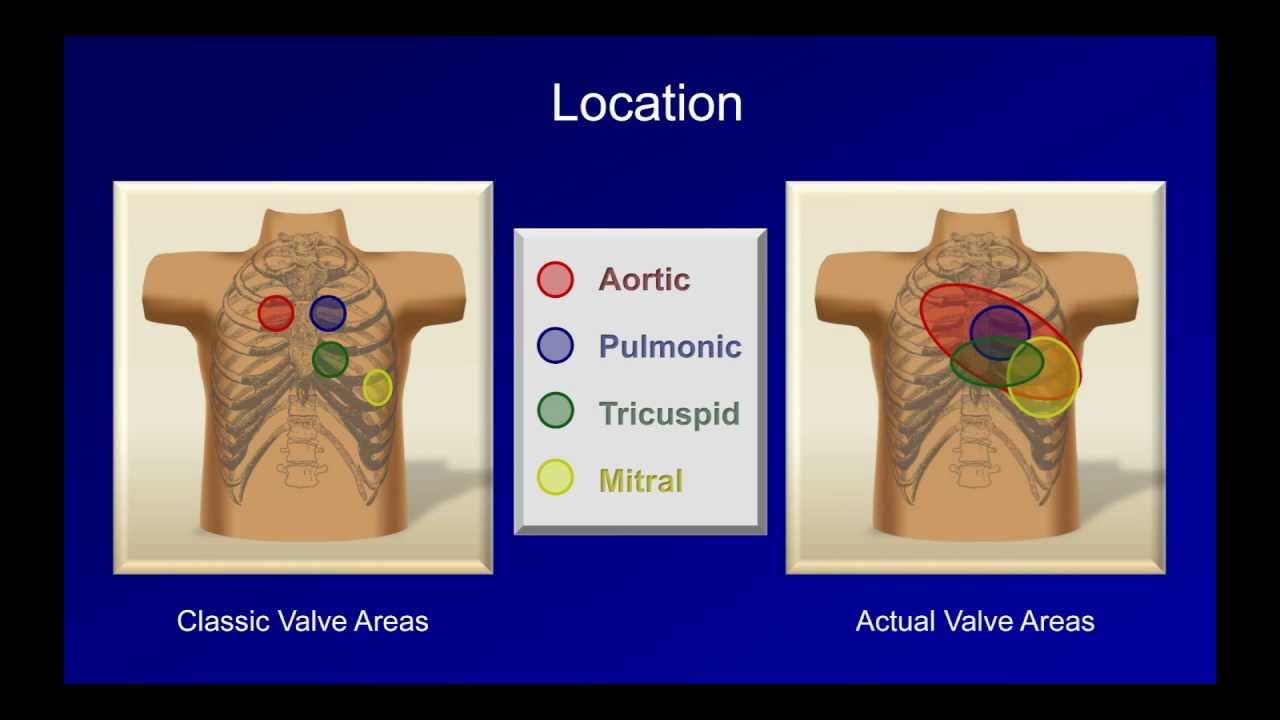
right all right that covers the heart sounds now let's talk about heart murmurs all right my friends so now we have to talk about murmurs when a patient has a heart murmur right so you've gone through you've said okay let me do the auscultate I hear S1 I hear S2 I don't hear any S3 S4 no real weird splitting of the S2 but here's something super odd in a particular area one of the first things that you have to do is know where you're supposed to be auscultating first thing where's the murmur that we actually
auscultate so we go there we grab our stethoscope and we say oh right secondary call space aortic area that could be associated with aortic stenosis so start thinking about that right away second intercost is based on the left side pulmonic area think about pulmonic valve diseases left third intercostal space think about aortic regurgitation and HCM left fourth intercal space tricuspidary think about a vsd left fifth intercostal space usually on the midclavicular line think about any mitral valve disease stenosis regurgitation and prolapse so right away if you hear those locations think about the possible types of
diseases that you will actually have occurring there so once you've gone through each particular location and you hear a murmur let's say that you hear a murmur in a particular location then you have to ask yourself the question okay is it a systolic diastolic or continuous murmur that's important so we're going to go through that now four systolic murmurs you are hearing it between S1 and S2 so when you listen to these you want to be able to use the particular terminologies of how they describe like the quality of the murmur or the characteristics of
the murmur when you hear a murmur that's referred to as a crescendo de Crescendo systolic murmur this is two typical typically two particular types of pathologies that are usually classic of what we call a crescendo de Crescendo murmur so it sounds really loud initially and then it decreases in intensity as you go on two particular murmurs one is there's a pathology with the aortic valve so we refer to this one as aortic stenosis so in aortic stenosis what happens is is it's really hard for blood to be able to get from the left ventricle out
into the aorta and what happens is his blood is trying to move through this area it kind of like bends these valves a little bit and it kind of bows them and when it bows them it produces this click and that's usually one differentiating factor between these two types of murmurs as you'll hear like this what's called an ejection click and then a crescendo decrescendo murmur that's classic for aortic stenosis the other thing is that this murmur is usually right upper sternal border so that right second intercostal space and it radiates usually to the carotids
and that's another particular thing that you can help to differentiate between this next one that I'm going to talk about this other one is Crescendo de Crescendo but it doesn't have an ejection click this one is usually due to the left ventricular outflow tract being super super narrow and obstructed this is called hypertrophic and sometimes they insert in the O obstructive but I'm going to put hypertrophic cardiomyopathy but it's a type of left ventricular outflow tract obstruction and what happens is it is really hard for blood to squeeze through this tiny little area from the
left ventricle and into the aorta but there's nothing that's actually causing a valve to bow or bend or anything like that that precipitates this click so there's no click but it is louder in the beginning and decreases as you go throughout systole this one though again usually her particularly around for the most part usually kind of like Herb's point is the common area for this one so you usually hear this around herbs point and this one doesn't usually have any radiation to the carotids so that's one real big thing so that's how you're going to
differentiate these two types of murmurs location timing and maybe some extra heart sounds and radiation okay cool the next one here is it's not a crescendo so let's actually mod like denote that it's a crescendo de Crescendo Crescendo de Crescendo murmur another big thing here is we have another one and this murmur is super interesting what happens is is you hear a murmur sometimes and it's usually pretty like it doesn't change an intensity throughout the systolic process but usually what happens is blood and this disease well normally during Sicily you're supposed to pump blood out
this way but there's a defect within this valve and this valve is supposed to block the mitral valve is supposed to block blood from going back into left Atria what happens is the valve buckles and it bends and when it bends it opens up this opportunity for blood to kind of Squirt back here into the left atrium which produces this regurgitation but you'll hear this click sound that actually comes about right before the actual murmur takes place and so this is called a ejection click and then this one right here this is called we're going
to put Holo a hollow systolic murmur usually what that refers to is it means that you hear it throughout the entire process of assistively but it's not technically the case because it depends upon where the ejection click occurs so sometimes this ejection clip can move so it can occur earlier and usually scenarios where the patient is super let's say having a very low venous return or it can come a lot later if you increase the advancement so we'll talk about Maneuvers that affect that later all right but that's the concept here now if you look
at these other two if we come down here same concept here so again we're going to have a patient here who has what's called a mitral valve prolapse so we'll say this one is a mitral valve prolapse they may have a regurgitating murmur associated with it another patient may have the same thing but this may again occur throughout the entire so this is truly what we refer to as more of a hollow systolic murmur so we're going to put here again this is definitely more classic of what we would use that term of holocystolic you're
hearing it throughout the entire process sometimes they say pan systolic holocystolic same thing but it's occurring between S1 and S2 continuously this is because during systole blood is supposed to go from the left ventricle into the aorta but all this blood during the immediate part of Sicily floods right back into the left Atria this is true mitral regurgitation so if a patient has mitral regurgitation there will be no click unless they have a prolapse of the actual valve and then regurgitation all right big thing to remember is both of these can be heard at the
Apex this one has a click this one does not have a click but it also can be heard of the Apex the other thing is that this usually radiates it radiates and if you listen at the fifth intercostal space you go over here you might be able to hear it in the axilla so sometimes this may also radiate to the axilla so that's one way that you can help to differentiate between these two but then there's one more another one is where you again can hear this murmur and it appears to sound holosystolic or pan
systolic so you hear it throughout the entire systolic process this one is again when we say holosystolic it's because of a vsd so we had mitroval prolapse mitral regurgitation and what's called a vsd now the vsd is usually particularly heard more likely around that fourth intercostal space so if you really wanted to you could add it you'll hear this on the left fourth intercostal space but what happens is the moment Sicily occurs blood is supposed to go from the left ventricle into the aorta the blood will jet over here into the right ventricle so the
smaller the hole is the louder the murmur is generally the larger the hole the softer the murmur is that's just because of like the actual turbulence of blood flow but in that concept here whenever this happens is going to be out throughout the entire systolic process one of the big things is location all right that's going to be one of the key things here and we'll also talk about Maneuvers so this is the ways that I want you guys to think about a systolic murmur is occurring between S1 occurring between S2 think about location think
about this extra heart sounds added on and think about radiation and then again use your terminologies to differentiate the quality or characteristic of the murmur all right cool deal one quick thing before we move on I mentioned pretty much all leftover heart murmurs right it doesn't seem like I mentioned many right heart murmurs the reason why is left is the ones that we're more concerned with right or less common plus guess what aortic stenosis and pulmonic stenosis will have the same type of quality of murmur it'll just be a different location mitral regurgitation and tricuspid
regurgitation will have the same type of murmur it'll just be a different location and so that's the big things to be able to understand the difference about cool diastolic murmurs what does that mean that means that these murmurs are occurring between S2 and S1 it's occurring after diastole or during diastole I should say so in this particular scenario we don't have any murmur between S1 and S2 is coming after S2 this one's interesting what happens in this one is you'll hear this murmur and it'll be the same between these two they'll look exactly the same
in configuration and it looks like it's decreasing in intensity as you go throughout diastole right this is called a decrescendo type of murmur all right what's the difference between these two all right in this one the patient has what's called aortic regurgitation and again it'd be the same concept if they have pulmonary regurgitation they would have a decrescendo murmur in this particular scenario blood will be jetting backwards during diastole blood supposed to come back but it gets blocked by the aortic valve if the aortic valve is damaged it'll jet back in and precipitate turbulence of
blood flow precipitate a murmur in this scenario for aortic regurgitation where would you generally hear this it's usually around that left uh third intercostal space we refer to this as herbs point so you should be able to hear this around herbs point right if it was pulmonic regurgitation it'd be a little bit different right so that's usually around like again usually more of like that left secondary causal space rather than the left third intercostal space so now that's one particular point the next thing here is that in this other disease this is mitral stenosis so
this is called mitral stenosis what happens in mitral stenosis is this valve is so thinotic and it's really difficult to get blood from the left atrium into the left ventricle super difficult and what happens is is as you're trying to push blood through here these valves will start to kind of like Buckle if you will and they kind of buckle at a certain point which kind of gives them this weird sound as you're trying to squeeze blood through this small area here they precipitate a kind of a clicking sound or a snapping sound and that
happens right here before the bakrescendo murmur you know what they call this an opening snap we're going to put o s so you'll hear this opening snap at the apex of the heart then a day Crescendo murmur that comes after that one that's classic of mitral stenosis so if I say opening snap Dickerson a murmur Apex mitral stenosis if I said herbs point a decrescendo murmur that was auscultated you would say this is a Aortic regurgitation type of murmur all right so we got these down same concept would exist if I were to say different
location for pulmonic regurgitation different location for tricuspid stenosis but same type of quality characteristics of the murmur and same timing of the murmur we come down to the last one the last type of murmur here is going to be a continuous murmur this is usually seen in the Pediatric population what happens with this one is that they have this murmur that usually is occurring between S1 and S2 and continues after S2 and the characteristic terminology behind this one is continuous but they add in something it's machine like so it sounds like it's a machine like
murmur and whenever you hear that terminology you want to think about a particular disorder called a PDA a patent ductus arteriosus what's happening in this particular murmur is blood is supposed to move left ventricle into the aorta and flow through the aorta but the left side heart pressures are generally higher than the right heart pressures and babies that are already born so naturally where will this blood flow it'll flow this way during systole then the heart will go into diastole so blood is supposed to kind of flow back shut that aortic valve closed but what
do you think about the aortic pressures during diastole in comparison to the pulmonary pressures during diastole it's still higher so regardless blood will keep shunting from the aorta into the pulmonary artery during both systole and diastole that's why it's continuous well one of the weird things is that this one is usually located around What's called the left infra clavicular area so this one is not a part of that classic locations that we uh kind of annotated prior so this is the way that we would Define murmurs in a very simple concept also take the locations
remember ape TM right from there oh you hear a murmur what is the timing is it systolic if it's systolic is it Crescendo de Crescendo or is it Holo does it have a click before or does it not have a click where is it again location and does it radiate that should help you oh it's not so solid it's diastolic okay does it have a decrescendo pattern oh it does does it have a CL opening snap that comes before or not and what's the location that's the key ways of differentiating and lastly is it a
continuous one usually continuous one is the easiest one to be able to pick out because it's the only one we have here and that's usually associated with PDA from there if you're still stuck with saying I don't really know the type of actual murmur it is then we can come to the Big Daddy we say okay I'm struggling between determining what kind of murmur this is I'm going to do specific Maneuvers to see if I can increase the intensity or decrease the intensity of the murmur and that may add to my confidence that this is
the type of murmur and if after all of that you're still not sure the classic thing that we usually go to is an echocardiogram to really Define the type of murmur all right let's start talking about the Maneuvers now to determine the type of mirror we get to the point where we say Okay location it's systolic versus diastolic then we can say what is actually happening if I do this particular position change this is really important to memorize one inspiration any right side murmur we didn't talk about the right side murmurs here because they're not
commonly tested but it's the same exact concept any right side murmur will be increased in intensity during inspiration because you're increasing the right side venous return any left-sided murmur would be decreased because you're not improving the venous return on that side that would be a one helpful sign expiration you're increasing the left side venous return and decreasing the right side of minutes return so the right side of murmurs will be decreased with expiration and left side murmurs increase with expiration straightforward if I lean forward it brings the aortic valve closer to the chest wall so
it'll increase the intensity of all aortic murmurs if I have them in the lateral decubitus position so I lay them on their left side and I listen there it'll bring the mitral valve closer to the chest wall so it'll increase the intensity of all mitral valve murmurs here's the big stuff if I increase venous return I have them squat I have I lift their legs up I'm increasing the venous return to the heart increasing venous return will increase the intensity of all murmurs except two it'll increase the intensity of all murmurs except two which are
hypertrophic cardiomyopathy and mitral valve prolapse it'll bring the the actual mitral valve prolapse remember there's a click and then a murmur it'll bring the click later and make the murmur shorter and it'll also decrease the intensity of the hypertrophic cardiomyopathy murmur if you do the opposite here which is decrease the venous or new balzava which increases the intrathoracic pressure and reduces venous return or you stand which reduces venous return that'll decrease the intensity of all murmurs except what mitrobot prolapse and hypertrophic cardiomyopathy in this it'll actually increase the intensity of HCM and then what it'll
do is in this scenario here from mitral valve prolapse you have to think about it it's actually going to cause the click to come earlier and then the actual murmur after that to be much longer and that's the big thing to remember okay next one is afterload when you increase afterload you're squeezing these hand grips and what this will do is this will increase the intensity of an aortic regurgitation murmur and mitral regurgitation murmur and it'll decrease the intensity of an aortic stenosis mitral valve prolapse and HCM murmur for decreasing afterload this is going to
be using things like ammo nitrate and super short acting it'll dilate the vessels if it dilates them it's going to do the opposite it's going to decrease the aortic regurgitation of micro regurgitation remember and increase the aortic stenosis and mitral valve prolapse and HCM armor the whole concept behind this is if you increase afterload the pressure inside of the order it's going to shoot blood back into the actual ventricle and also make it easier for blood to fly back into the left atrium that's why it'll increase these murmurs if you decrease the afterload the blood
won't be shooting back into the ventricle and shooting back into the Atria that's why it decreases in this types of murmurs for aortic stenosis mitrobot prolapse and HCM again if you increase the afterload here what you're doing is you're making it harder for blood to leave the left ventricle and move out into the aorta that's going to decrease the flow across the aortic semilunar valve decreasing aortic stenosis that'll decrease the buckling of the mitral valve decreasing that click and then murmur and also it'll actually help because what it'll do is when you increase after that
we'll talk about this a little bit later but it keeps more blood in the left ventricle and stretches out the left ventricle and flattens out that septum and reduces the obstruction there in HCM but that's the concepts I need you guys to remember [Music] all right my friends we covered aortic diseases I hope that made sense I hope that you guys enjoyed it and as always until next time foreign [Music]