Understanding Peripheral Arterial Disease
263.59k views2192 WordsCopy TextShare
Zero To Finals
This video contains a visual explanation of peripheral arterial disease, aimed at helping students o...
Video Transcript:
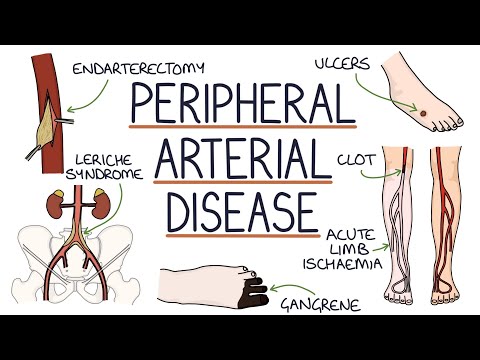
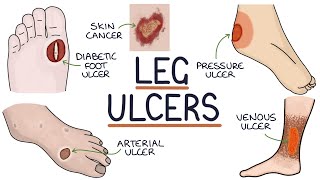
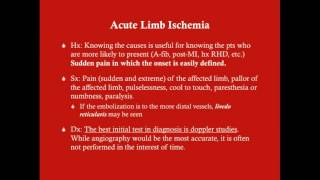
foreign [Applause] [Music] ers. com in this video I'm going to be going through Peripheral arterial disease and you can find written notes on this topic at xerodifinals. com pad or in the vascular surgery section of the zeroid finals surgery book so let's jump straight in Peripheral arterial disease refers to the narrowing of arteries supplying the limbs and the periphery which reduces the blood supply to these areas it usually refers to the lower limbs resulting in symptoms of claudication intermittent claudication is a symptom of ischemia in a limb which occurs during exertion and is relieved by rest it's typically a crampy achy pain that occurs in the calf thigh or buttock muscles and is associated with muscle fatigue when walking Beyond a certain intensity critical limb ischemia is the end stage of Peripheral arterial disease where there is an inadequate supply of blood to a limb to allow it to function normally at rest the features are pain at rest non-healing ulcers and gangrene there is a significant risk of losing the limb acute limb ischemia refers to a rapid onset of ischemia in a limb typically this is due to a thrombus or a clot blocking the arterial supply of a distal limb similar to a thrombus blocking a coronary artery in a myocardial infarction it refers to inadequate oxygen supplied to the tissues due to reduced blood supply necrosis refers to the death of tissue gangrene refers to the death of tissue specifically due to an inadequate blood supply let's talk about atherosclerosis atherary refers to soft or porridge-like and sclerosis refers to hardening atherosclerosis is a combination of atheromas which are fatty deposits in the artery walls and sclerosis which is the process of hardening or stiffening of the blood vessel walls atherosclerosis affects the medium and large arteries it's caused by chronic inflammation and activation of the immune system in the artery wall lipids are deposited in the artery wall followed by the development of fibrous atheromatous plaques these plaques cause stiffening of the artery walls leading to hypertension or raised blood pressure and strain on the heart whilst it tries to pump blood against increased resistance the plaques also cause stenosis leading to reduced blood flow for example in angina and they can lead to plaque rupture resulting in a thrombus that can block a distal vessel and cause ischemia for example in acute coronary syndrome let's talk about the risk factors for atherosclerosis it's important to break the risk factors down into modifiable and non-modifiable risk factors we can do nothing about the non-modifiable risk factors but we can do something about the modifiable ones the non-modifiable risk factors for atherosclerosis are older age family history and being male the modifiable risk factors are smoking alcohol consumption a poor diet which is high in sugar and trans fat and low in fruit vegetables and omega-3s a sedentary lifestyle with little exercise obesity poor sleep and increase stress let's talk about medical comorbidities medical comorbidities increase the risk of atherosclerosis and should be carefully managed to minimize the risk and these include diabetes hypertension chronic kidney disease inflammatory conditions such as rheumatoid arthritis and the use of atypical antipsychotic medications for example in schizophrenia a Time tip for you think about the risk factors when you're taking a history from someone with suspected atherosclerotic disease such as someone presenting with intermittent claudication ask about their exercise diet past medical history family history occupation smoking alcohol intake and medications this will help you perform well in exams and when you're presenting to seniors as you'll be able to classify them as high risk or low risk for having the condition that you're suspecting there are several end results of atherosclerosis these include angina myocardial infarction transient ischemic attacks Strokes Peripheral arterial disease and chronic mesenteric ischemia let's talk in more detail about intermittent claudication Peripheral arterial disease presents with intermittent claudication patients May describe a crampy type pain that predictably occurs after walking a certain distance after stopping arresting the pain will disappear the most common location is the calf muscles but it can also affect the thighs and buttocks next let's talk about critical limb ischemia the features of critical limb ischemia can be remembered with the six piece mnemonic and these six P's are pain palour pulseless paralysis paresthesia which is an abnormal sensation or pins and needles and finally perishingly cold critical limb ischemia typically causes a burning pain and this pain can be worse at night time when the legs are raised up on the bed as gravity no longer helps to pull blood into the foot next let's talk about a very specific syndrome called Larice syndrome Larice syndrome occurs with occlusion in the distal aorta or proximal common iliac artery and there's a Triad of thigh or butter claudication absent femoral pulses and male impotence so if you see this Triad in your exams think of Larice syndrome next let's talk about the signs of Peripheral arterial disease on examination you can look for the risk factors for Peripheral arterial disease such as tar staining on the fingers which can indicate smoking and xanthamata which are yellow cholesterol deposits on the skin indicating hyperlipidemia you can look for signs of existing cardiovascular disease such as missing limbs or digits after previous amputations for critical limb ischemia midline sternotomy scar which can indicate a previous coronary artery bypass graft a scar on the inner calf for saphenous vein harvesting which may indicate a previous coronary artery bypass graft and focal weakness which may suggest a previous stroke the peripheral pulses may be weak on palpation palpable pulses throughout the body are the radial brachial carotid abdominal aorta femoral popliteal behind the knee posterior tibial and dosalis pedis pulses a handheld doppler can be used to accurately assess the pulses when they're difficult to palpate the signs of arterial disease on inspection are skin power cyanosis dependent rubor which is a deep red color when the limb is lower than the rest of the body muscle wasting hair loss ulcers poor wound healing and gangrene which is the breakdown of skin and a dark red or black change in coloration on examination there may be reduced skin temperature reduce sensation to the skin a prolonged capillary refill time of more than two seconds and changes during Burger's test let's talk in more detail about Burger's test Burger's test is used to assess for Peripheral arterial disease in the leg there are two parts to the test the first part involves lying the patient on their back or supine lifting the patient's legs to an angle of 45 degrees at the hip one at a time holding them in that position at 45 degrees for one to two minutes looking for power in the leg if the leg goes pale this indicates the arterial Supply is not adequate to overcome gravity and this suggests Peripheral arterial disease Burger's angle refers to the angle at which the legs turn pale due to an inadequate blood supply for example a Burger's angle of 30 degrees means that when the leg is held at 30 degrees it goes pale the second part of the test involves sitting the patients with their legs hanging over the side of the bed blood will flow back into the legs assisted by gravity in a healthy patient the legs will remain a normal pink color in a patient with Peripheral arterial disease they will go Blue initially as the ischemic tissue deoxygenates the blood and then a dark red after a short time due to vasodilation in response to the waste products of anaerobic respiration the dark red color is referred to as rubor next let's talk about leg ulcers leg ulcers indicate the skin and tissues are struggling to heal due to an impaired blood flow some features help you distinguish between arterial and venous ulcers arterial ulcers are caused by ischemia secondary to an inadequate blood supply typically arterial ulcers are smaller than venous ulcers deeper than venous ulcers have well-defined borders which gives them a punched out appearance occur more peripherally for example on the toes have reduced bleeding and are painful venous ulcers are caused by impaired drainage and the pooling of blood in the legs typically venous ulcers occur after a minor injury to the leg they're larger than arterial ulcers they're more superficial than arterial ulcers they have an irregular gently sloping border they affect the gator area of the leg which is from the mid calf down to the ankle they're less painful than arterial ulcers and they occur with other signs of chronic venous insufficiency for example hemosiderin staining and venous eczema next let's talk about the investigations for Peripheral arterial disease and these include an ankle brachial pressure index or abpi duplex ultrasound which is an ultrasound scan that shows the speed and volume of blood flow and angiography which can be a CT or MRI angiogram and this involves using contrast to highlight the arterial circulation let's talk in more detail about the ankle brachial pressure index the ankle brachial pressure index or abpi is the ratio of this histolic blood pressure in the ankle around the lower calf compared with the systolic blood pressure in the arm these readings are taken manually using a Doppler probe for example an ankle systolic blood pressure of 80 and an armed systolic blood pressure of a hundred gives a ratio of 0.
8 which is 80 divided by a hundred the ankle brachial pressure index results can indicate the severity of Peripheral arterial disease a result of 0. 9 to 1. 3 is normal 0.
6 to 0. 9 indicates mild Peripheral arterial disease a ratio of 0. 3 to 0.
6 indicates moderate to severe Peripheral arterial disease and a ratio less than 0. 3 indicates severe disease to critical ischemia an ankle brachial pressure index above 1.
Related Videos
9:39
Understanding Leg and Foot Ulcers
Zero To Finals
223,934 views
43:06
Peripheral Arterial Disease | Clinical Med...
Ninja Nerd
28,499 views

8:21
Peripheral Arterial Disease & Peripheral B...
Level Up RN
81,256 views

8:35
Understanding Varicose Veins
Zero To Finals
467,493 views
24:51
Acute Limb Ischemia - CRASH! Medical Revie...
Paul Bolin, M.D.
48,148 views

46:52
Walking and Peripheral Artery Disease | Dr...
The Way To My Heart
26,209 views
5:00
PAD vs. PVD | Peripheral Arterial Disease ...
NurseInTheMaking
86,752 views

16:39
Peripheral Arterial Disease: Symptoms, Ris...
Talking With Docs
30,417 views

12:53
Understanding Deep Vein Thrombosis (DVT)
Zero To Finals
411,946 views

10:51
Peripheral Vascular Examination - Clinical...
Dr James Gill
652,514 views

52:22
Coronary Artery Disease | Clinical Medicine
Ninja Nerd
154,828 views
![How To FIX Blood Flow & Circulation! [Heart, Arteries, Legs & Feet]](https://img.youtube.com/vi/HwcfPwxrL-A/mqdefault.jpg)
20:26
How To FIX Blood Flow & Circulation! [Hear...
Michigan Foot Doctors
1,390,548 views

16:45
Understanding Gallstones
Zero To Finals
278,892 views
4:23
PAD vs PVI cartoon animation & memory tr...
SimpleNursing
1,175,392 views

59:33
Peripheral Artery Disease - Is There a Hol...
Stanford Health Care
95,420 views
24:16
Understanding The Causes of Pain and Pain ...
Zero To Finals
182,027 views
7:05
Peripheral Vascular Examination - OSCE Gui...
Geeky Medics
316,220 views
41:56
Hypertension | Clinical Medicine
Ninja Nerd
186,678 views

5:53
Peripheral vascular disease, Causes, Signs...
Medical Centric
89,692 views
6:18
Understanding Chronic Venous Insufficiency
Zero To Finals
313,332 views