Cardiovascular | Electrophysiology | Intrinsic Cardiac Conduction System
1.59M views8690 WordsCopy TextShare

Ninja Nerd
Official Ninja Nerd Website: https://ninjanerd.org/
Ninja Nerds,
In this lecture Professor Zach Mur...
Video Transcript:
all right engineers in this video we are going to talk about electrophysiology this is an extremely important topic and the reason why is because the heart is so special it has the ability to intrinsically depolarize itself it doesn't really depend upon the nervous system we'll talk about how the nervous system like the extrinsic inovation of the heart can speed up the heart rate or decrease the heart rate as well as maybe even increase the contractility of the heart we'll discuss these things but again I want you to understand something about the heart the heart exhibits
what's called automaticity what is automaticity so the heart exhibits a a very important characteristic and this very very important characteristic is called automaticity what is automaticity automaticity is basically the heart has its the intrinsic ability on its own to spontaneously deep polarize itself and then Trigger action potentials to send it out to all the other parts of the heart that is automaticity so one more time automaticity is the intrinsic ability of the heart to spontaneously depolarize and Trigger action potentials that are spread out all the entire myocardium the muscle layer of the heart to trigger
the heart muscle to contract okay that is its intrinsic ability how does this happen let's get started on that so what I'm doing is I'm zooming in here on some cells so before we get into all that Nitty Gritty components of the cells I want to take a look at the larger kind of like gross structure of this so let's come over here to this big old heart so in the heart you're going to have two different types of components of The myocardium so when you look at The myocardium you have two parts so when
you look at The myocardium it's actually broken up into two components one is it's broken into what's called nodal cells which are basically your non-contract house these are the ones that generate automaticity these are the ones that can spontaneously depolarize generate Action potentials so they don't contract these for to name a few is going to be like the SA node which stands for sinoatrial node AV node which stands for atrio ventricular node the AV bundle which is the atrio ventricular bundle sometimes you might even hear it referred to as the bundle of His and there's
also going to be What's called the bundle branches and you have one bundle branch going to the right side of the heart one bundle branch going to the left side of the heart so for your bundle branches you have both a left and a right and you have these very specialized structures that are digging into very very small components of The myocardium and these are called your preni fibers so again with The myocardium there's two types of tissue one is these nodal cells and the noal cells are non-contractile cells they're the ones that can intrinsically
depolarize generate action potentials and Trigger the contraction of the heart these are SA node AV node AV bundle or bundle of hiss right and left bundle branches and your peni fibers the other component of The myocardium is the contractile cells so these are the ones that consist of the actual contractile proteins these are the ones that consist of actin and mein and they consist of uh the you know the troponin and the tropomyosin we could just keep going on right they consist of a lot of these contractile proteins what else they're the one that actually
consist of the sarcoplasmic reticulum so they consist of that very specialized structure called the sarcoplasmic reticulum so with that said two parts of The myocardium nodal cells and contractile cells the ones that are Contracting they make up the big big portion of the heart these are the ones that consist of these contractile protein units as well as psychop plasmic ium they're the ones that generate the force that pushes the blood out of the heart the nodal cells are the ones that set a rhythm or a pace where does this whole pacing or automaticity start and
where can you find all these structures within the heart well you got to look right at the actual pacemaker of this actual cardiovascular system now that we know that the myocardium is made up of two different types of cells nodal cells and contractile cells we want to focus on these guys first these nodal cells where can you find these bad boys well we got to look at at the pacemaker we got to look at the one who's actually generating the heart rhythms or the sinus rhythm that's this guy he's actually located right here so what
do we call this guy here he is called the SA node This Guy's super important where would you actually find him you're going to find him if we look here at the orientation of the heart this is your right atrium right this is the right ventricle this is the left ventricle and this is the left atrium so if you look into the right atrium right here you're going to find in the superior component of the right atrium just beneath this large vessel here called The Superior vnea you're going to find this crescent-shaped structure consisting of
nodal cells that is called the SA node the SA node is the pacemaker he sets What's called the sinus rhythm now sinus rhythm for the SA node is generally he sets the pace at around 60 to about 80 uh beats per minute now that's really important because when we have this type of pace that's the normal heart's ability so the heart can generate about 60 to 80 beats per minute on its own without any extrinsic inovation okay without any autonomic nervous syis so no sympathetic effect no parasympathetic effect this is what it can generate on
its own so this normal Pace that we're setting here around 60 to 80 beats per minute this is called your sinus rhythm okay so it's called your sinus rhythm okay that's your sinus rhythm so sinus rhythm is generated by the SA node where it's generating Action potentials right about 60 to 880 to trigger this actual heart to beat 60 80 times per one minute okay that's the normal Sous Rhythm now we're going to talk about how it generates Action potentials but before we do that we need to see where these Action potentials are getting sent
to we need to know the normal conduction pathway so this guy is the one that's generally setting the pace when he sets this pace he sends this information from the right atrium into the left atrium how does he do that you know there's a specialized structure over here that's connecting the essay note over here to the left atrium kind of like a little special structure over here kind of spreads out like this it's coming from over here this right here is called the Bachman's bundle okay it's called Bachman's bundle so this is called Bachman's bundle
and what happens is is these electrical potentials that Theo generates he can send some of these electrical potentials over here through Bachman's bundle to activate depolarize the Atria so Isn't that cool so you can send action potentials from the sa no which is in the right atrium over to depolarize the left atrium via Bachman's bundle another thing is we have to connect this SA node here to other parts of the Atria so we have to connect to other parts of the Atria so there's other parts here that can come and Supply different parts of the
Atria here like this what is these guys here this is actually called the internodal pathway so all of these guys here will come out and stimulate different parts of the Atria and eventually converge onto that big structure right there but again what are all of these fibers right here that are coming from the essay node outward to all the other parts of the left atrium all of these fibers here like this one and this one and this one these are making up what's called your inter nodal pathway so saay note to Bachman's bundle is going
from the right atrium to the left atrium to supply the left atrial myocardium from the SA node to these internodal Pathways this will supply all the other parts of the right atrium but eventually all of this internodal pathway will converge onto this second important structure what is the second important structure called this second important structure is called the AV node okay it's called The Av node the AV node is so important because look what he's doing so he's kind of peing underneath this actual uh pulmonary trunk here it's actually running from the actual right atrium
and into the actual this whole thing right here what is this big structure right here if you guys watched the video on the structures and layers of the heart you know that this would be the interventricular septum right so that's the interventricular septum what happens is this bundle here this AV node runs from the actual right atrium into the interventricular septum so it's acting as a connection the Gateway between the Atria and the ventricles because what happens is some of these potentials from the Bachman's bundle can actually make their way over here to the AV
node also so some of the action potentials from the Bachman's bundle can make their way over here to the AV node so either way all of the action potentials that are coming from the SA node that are being spread out for the interal pathway or the Bachman's bundle are converging onto the AV node once the AV node receives these signals it's going to take a little bit of time how long it the actual action potentials here take about 0.1 second about 0.1 seconds which is a little bit longer than how much it takes for them
to move through the SA node cells the Bachman bundle cells the internodal pathway cells so because it takes a long time what's the significance of this because it has significance one of the significance allowing for the AV node to take a 0. one second delay before it sends the action potentials down through the interventricular septum to the bundle of hiss is because it wants to give time for Atria to contract before the ventricles contract I can't express how important this is because of this 0.1 second delay it gives the time enough adequate time for the
Atria to contract and push their blood into the left ventricle because if the AV no were to fire not have that1 second delay it would it' be depolarizing The myocardium while the left atrium and right atrium are trying to empty their blood into the ventricles if that's the case then as the ventricles are getting depolarized they might start Contracting at the same time that the Atri are Contracting that's counterintuitive we don't want that we want to allow for this guy to contract squeeze all the blood into the ventricles then let the ventricles attain the blood
and then squeeze the vent squeeze the ventricles to push it out through the aorta and the pulmonary circulation okay now question is why does it take 01 second we know that it's the purpose it gives the time for the Atria to contract before the ventricles contract but there's two microscopic reasons why these nodal cells are riddled with a ton of Gap Junctions which are just basically channels that allow for ions to pass from cell to cell however the AV node which consists of a bundle of those nodal cells it has a lot fewer Gap Junctions
than these other nodal cells so a lot less Gap Junctions so a lot less ions can flow from cell to cell that decreases the ual speed at which it's moving that's one reason that's why it takes a little bit longer another one is because they have a smaller diameter so the actual fibers are actually a lot smaller in diameter and if you know a little bit about conduction we know that the larger the diameter of the structure the faster the velocity of that conduction is going to move so the smaller the diameter the slower the
conduction speed okay so again we went from SA node which was the first one through the Bachman's bundle internodal pathway into the AV node AV node was the second one took 01 second delay to give the time for the Atria to contract empty their Chambers so that the ventricles can attain the blood and then they can contract why does it take the 0.1 second delay because the AV node has less Gap Junctions and it has fewer D smaller diameter muscle fibers okay then where does it go from here it goes into the next structure here
this next structure here is going to be kind of like a nice bundle it's consisting of a big old bundle right here this guy right there is called the bundle of hiss okay so this guy right here is called the bundle of His or the AV bundle when he receives these Action potentials from The Av node he then conducts it into these two bundle branches this bundle branch right here we're going to put here four is going to the right myocardium so this is the right bundle branch so which one would this one be right
bundle branch over here this is going to the left myocardium so because this is going to the left myocardium what we say this one is this is the left bundle branch because it's going to left myocardium then from there it goes into these nice little breaking units you see how this is branching off branching off branching off branching off these bundle branches these are called your preni fibers okay so these are your preni fibers okay these are your peni fibers all right so let's go ahead and recap these let's recap them in order now I'm
about to get a little taller okay don't you dare laugh at me I'm short all right so let's go ahead and recap the flow so how does it go we said first things first started at the SA node he's the pacemaker of the respiratory I'm sorry the pacemaker of the actual cardio Cardiovascular Center right specifically for this actual Pace setting of the heart rate then what happens he goes to the next one how does he get to this next one he goes to the AV node how does it get to the AV node remember it
travel within the actual right atrium via the internal pathway but then the SA node can transmit impulses to the left atrium via the Bachman's bundle eventually all of those fibers converge onto the AV node though the AV node we said takes about a 0.1 second delay because of the fewer diameter uh fibers and less Gap Junctions and to allow for the Atria to contract and then the ventricles to contract then from The Av bundle we go to the bundle of His or again you can call it the AV bundle doesn't matter from there it goes
into the right and left bundle branches okay so we're just going to combine these you can go into the right and left bundle branches if it's the right one it's going to the right myocardium if it's the left bundle branch it's going to the left myocardium then from here you're going to go into the last one which is going to be the pereni system so the pereni fibers and this will supply different components within The myocardium and Trigger The myocardium to contract we did that now so now we've covered the actual cardiac conduction system okay
sweet from there now what are we going to do we now now we know the cardiac induction system the actual gross anatomy like flow but now we got to be even more specific how does it generate these Action potentials how does it actually do it so now what we're going to do is we're going to do two things I'm going to take this sa noal cell I'm going to take out out of this sa no I'm going to take and expand on one of the cells then I'm going to take a piece out of the
myocard and I'm going to expand that and look at one cell so we're going to look at two different types of cells we're going to look at a nodal cell and we're going to look at a contractile cell and see how these cells are communicating and what's all these ion channels and stuff okay so let's go and get started so this cell right here let's actually just toote it right away this is our nodal cell okay this is going to be the nodal cell and this one over here just so we can get right out
of the way this is going to be the contractile cell now what did I tell you right away about the Cellular Connections we said these two cells okay because not only are nodal cells because look I could actually kind of make a tiny little mini diagram here I can say that if I have this nodal cell here this nodal cell could be connected to many other nodal cells and how could they be connected what are these little things that are connecting the nodal cells the actual Gap Junctions and so if I have Gap Junctions here
this can allow for ions to pass from this cell to this cell to this cell to this cell right it's basically allowing for ions to pass from cell to to cell the same thing happens and exists between let's say that this is a nodal cell and just to make it very simple I changed the color of the actual contractile cell I make the contractile cell black these also have connections so if these have connections we can actually allow for ions to flow from a noal cell into a contractile cell and then help the contractile cell
to start depolarizing so we're going to see how that happens but but first before we do that we got to see how does this guy depolarize itself so you know something funny within these noal cells very funny very very interesting little cells and they actually consist of what's called funny Sony sodium channels you think I'm being funny but I'm not there's actually funny sodium channels these channels that are within this nodal cell are very leaky and they allow for a little bit of sodium to leak into the cell very very slowly very very very slow
flow of this sodium into this noal cell now generally nodal cells don't have a stable resting membrane potential normally resting membrane potential is like -70 toga 90 MTS it depends upon the cell but these nodal cells don't really have a stable resting membran potential so their kind of membrane potential fluctuates but in general before these sodium channels uh these funny sodium channels open they generally are going to have a membrane potential around -60 molts that's approximately where it's at so now look what happens here let's let's represent these funny sodium Channels with blue these funny
funny sodium channels start actually causing the inside of the cell to become a little bit more positive because we're bringing positive ions into the cell sodium as the sodium starts coming into the cell something else really weird starts happening as you approach the threshold potential sodium gets a little bit of help okay so first things first was the sodium is coming into the cell bringing some positive charges with it all right this happens around 60 molts but then what happens is these other channels they're called ttype calcium channels these are called t types calcium channels
these calcium channels open up approximately around - 55 molts so these positive ions are bringing it from -60 Mill volts to what 55 because it's a really slow flow of sodium as it starts flowing in this 55 molts becomes a stimulus for these ttype calcium channels when they stimulate these ttype calcium channels start opening and calcium starts flowing in nice and slowly also so now we have the combined effect of these funny sodium channels what are these guys here called funny sodium channels these are your funny sodium channels these guys are slowly allowing for the
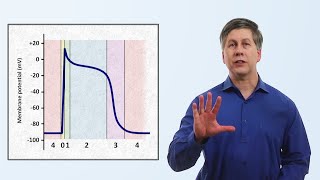
sodium minus to trickle in then what happens happens is it stimulates these ttype calcium channels to come in once they reach about 55 as these calcium ions start accumulating with the sodium ions guess what happens to the membrane potential it becomes even more positive let's show that down here so now if you look you're going to notice that this is going to be representing the calcium channels and the sodium channels look oh shoot they hit threshold potential what is our threshold potential here generally within the cell the threshold these actual nodal cells is around -40
Ms normally it's like 50 five in most cells but in this one it's about --4 once we hit that -40 another type of Channel opens up when this channel opens up it blasts open a lot of calcium and you're going to see what happens here that this guy actually Rises pretty quickly here it rises up very very quickly and we'll see what happens here in just a second okay so for right now I want you to know that whenever we're inside the cell 60 Ms funny sodium channels open then around 55 these uh ttype calcium
channels open then when we hit threshold what channels open these green channels what are these green channels here called these green channels are called L Type calcium channels so these are called your L Type calcium channels they're very very sensitive to voltage so once this happens it gets to around -40 Mill volts and guess who starts flowing in very powerfully calcium starts flowing in very very powerfully as the calcium starts flowing in in very very aggressively what would you expect to happen to the inside of the cell to become super super super positive and that's
what happens look it goes up to-4 and W shoots up how high does it go up to it generally goes up to approximately in this cell because the calcium is coming in very very very aggressively It generally comes in to approximately around positive 40 molts so it comes into about positive 40 molts as these L Type calcium channels open the calcium starts rushing in you're bringing a lot of positive ions into the cell and as you start bringing tons and tons and tons of positive ions into the cell what is it going to do to
the inside of the cell it's going to depolarize the cell so what's the overall result here well let's actually kind of follow what happened here if we look at this in kind of like a nice little flow diagram here 60 MTS was the resting membrane potential the funny channels open and we brought it to 55 mols right this was when we opened up T type calcium Chann but T calcium then we got it from that to threshold potential which is around 40 MTS this opened up L Type calcium channels then from that we took in
this L Type calcium channels when they open calcium flooded in so aggressively that it completely flipped the membrane from -4 to about posi 40 molts this is when it's depolarized so the inside of the cell is depolarized and extremely positively charged okay now we've depolarized the cell it didn't require any nervous system functioning isn't that beautiful now here's the thing how in the heck does that affect this actual contractile cell these beautiful Gap Junctions so what happens is is what are we accumulating a lot of inside of this cell lots and lots of positive charges
lots of cations ions so as a lot of these cat ions are being loaded into these uh into these actual nodal cells what can happen well guess what these beautiful Gap Junctions are connecting they're acting as the communication Gateway between the nodal cells and other nodal cells or the nodal cells and contractile cells so what do these Gap Junctions actually made up you know they're made up of what's called proteins uh specifically called conin so they're called conin proteins so there basically a whole bunch of different types of conin now these cat I they actually
move through these Gap Junctions into the other cells they can go from cell to cell to cell to cell to cell now because of that I'm bringing positive ions over into this cell through the Gap Junctions which is so darn cool but here's the thing how do we keep these cells so tightly close together so that the Gap Junctions aren't separating whenever the heart's being stretched because we don't want these actual Gap Junctions to get separated because it's actually two different proteins between the cells connecting together how do I actually prevent this from happening to
keep the cells so tightly together we have these special structural proteins here what is this what is this protein here called this protein here is called desmosome okay it's made it has what's called desmo zomes now desmosomes are super cool because they consist of a bunch of different proteins like for example these green proteins here that are connecting the cellto cell lying for the cellto cell communication these are called cadherin and then these proteins here these blue proteins these are actually your your attachment plaques and there could be many different proteins that make this up
it could be what's called um desmo plen there could be what's called uh other different types of chemicals we're not going to go into all of these different types I don't want to do that but there's many different types of proteins that are making up these attachment plaques okay then there's other proteins which are consisting of these other types of filaments here that are consisting of substances like Artin okay so we know that these desmosomes are basically acting as like adhesion molecules from cell to cell connecting the cells together keeping them very tightly connected that's
really really important now that leads to a concept whenever I have two cells communicating together and I have a combination of desmosomes and GAP Junctions they decided hey let's give it a different name like always right let's let's let's give this a name so they said it's actually right over here they said that whenever you take Gap Junctions and you add into the mix desmosomes they're like oh you know what let's call this inter collated discs so inter collated discs are just basically a bunch of Gap Junctions and a bunch of Desmos zones connecting the
actual cardiac cells together that's it so now again what will be happening over here a lot of cat ions sodium and and calcium ions are flowing through these Gap Junctions into this other cell this contractile cell how does this help the contractile cell all right let's see the cell starts becoming a little bit more positive right we'll see what happens whenever this cell relaxes in a second we'll do the relaxation period together let's keep going with the depolarization positive ions come over into this cell when the positive ions come over into this contractile cell we
have have to think about what is the actual resting membrane potential of this cell this one's a little weird this one was like -60 we said the resting membrane potential of this cell is right around 85 to 90 molts okay so its resting membrane potential is in between like 85 to 90 Mill volts okay so right around that now these positive ions those positive ions that are leaking into the cell via the Gap Junctions they start trying to bring the actual membrane potential closer towards the threshold that's what they're trying to do they're trying to
bring this closer towards threshold that's their purpose but what happens is along that way okay what's what's threshold potential within these cells threshold potential is approximately right around 70 Mill volts within these cells so you see how different cells can have different resting member potentials and threshold potentials it depends upon the movement of potassium ions okay and we'll talk about that when we talk about resting membrane potential with the nerd equation but what happens is these ions these cat that are flowing into the cell are bringing the resting membrane potential closer to threshold potential as
it does that we reach threshold and these specialized voltage gated sodium channels blast open let me see let me show you where these guys are so here are the positive ions what is it doing and originally the cell is at resting membrane potential it brings it to about threshold potential which is around -70 molts this stimulates these voltage G sodium channels these voltage gated sodium channels start opening when they open who starts flowing in sodium and when sodium Flows In he Flows In very very fast as the sodium lons start flowing into the cell the
inside of the cell starts becoming very very positive so it starts becoming very very positive as it becomes very positive this positive charge starts moving across the actual cell membrane or in this case what's the cell membrane of a muscle cell called It's called The ccma so these positive charges start moving in like a wave around the actual ccma of the muscle cell membrane so look at the graph what are we going to see we were originally at90 we went to 70 through those Gap Junctions hit threshold potential and opened up what channels those voltage
gated sodium channels and Rises up now it rises up kind of a little bit you know a little bit slower but um what happens is it gets to about positive around positive 10 molts so it gets to approximately around postive 10 molts now along the way along the way throughout this process you're approaching positive 10 molts some other channels open up a a little bit and allow for a little bit of calcium to start trickling in so along this way another thing that can happen is if we look over here these black channels these black
channels are calcium channels these are your calcium channels and along the way as the sodium is starting to approach and start causing the cell to depolarize some of these calcium channels start slowly opening only a little bit of them start slowly opening and calcium starts coming in too okay so start calcium starts kind of slowly trickling in also with the Sodium and this causes that Rising phase there there it gets to about positive 10 molts when it gets to positive 10 molts the sodium channels inactivate okay so they turn off so now the sodium channels
are closed but what else what other channels open a little bit a little bit of calcium channels are open very very little though not too many but what else decides to open up at the same time another channel that decides to open up at the same time over here is going to be pottassium these potassium channels they like ah you know what it's the perfect time for me to open up the cell is super super depolarized let me go ahead and open up a little bit because we're at positive 10 mols that can't happen we
got to bring it down a little bit so what happens is these potassium channels open up and they allow for pottassium ions to start coming out now the potassium ions start coming out a little bit more than the calcium ions are kind of slowly slowly trickling in so a lot of potassium ions are going to go out here for moment of time as that starts happening what starts happening to the inside of the cell it's losing positive charges it's becoming a little bit more negative what happens then because the pottassium leaks out of the cell
for a moment it drops down a little bit weird right has a little drop and it drops from about 10 molts to around zero so because of that because of that actual sodium ions coming in and a little bit of calcium trickling in it brings it up to posit 10 MTS at positive 10 sodium channels close potassium channels open and potassium starts slowly leaking out a tiny tiny bit of calcium is coming in and it causes it to drop down to around 0 molts when it hits Z molts the calcium channels those actual volt those
voltage calcium channels become even a little bit more active they become even a little bit more active now so once you hit about positive zero I guess there is no such thing as positive z z is positive no matter what you hit zero Mill volts that becomes a very powerful stimulus for these L Type calcium channels okay so these are your L Type calcium channels as these hit positive zero they become a little bit sensitive and the calcium starts flowing in very powerfully okay it starts coming in these positive ions from the calcium starts coming
into the cell but don't get that Twisted because guess what else is leaving out at the same time time just a little bit with it these potassium ions are also leaving the cell so because of that we're having potassium ions leave the Cell at the same time cat I calcium ions are coming into the cell so if you think about it positive ions are leaving and positive ions are coming in so really there's no change in the membrane potential well that's weird so what would that be then it's going to kind of plateau for a
little bit and it's going to Plateau actually for a decent amount of time about 250 milliseconds that's pretty long time for a cell okay to be in this depolarized or plateaued like state so to get this clear first things first we have this 90 to70 that's due to those actual uh c those Gap Junctions bringing the actual ions in to get us to the actual threshold to allow for the voltage G the sodium channels to open up then after that there's a little drop that little drop there is do the potassium channels open and more
potassium leaves out than calcium is coming in and it causes it to go to positive Z molts or zero molts once we hit zero those L Type calcium channels become a little bit more active open up and a little bit more calcium than normals coming in but because positive ions like calcium is coming in and positive ions like potassium are going out okay so it's going to Plateau then let me get some terms out of the way here just real quickly doctors I guess wanted to make it a little bit more complicated for us so
they added phases the phases that they actually ordered in it goes from zero to four so this depolarization phase where the sodiums are coming in they call that phase zero okay so phase zero is where the sodium ions are coming in very aggressively through the that depolarizing current the voltage gated sodium channels then this little dip down where the potassium channels open and the potassium starts leaking out to bring the membrane potential from positive 10 to zero mainly potassium very little calciums are coming in this is called phase one the plateau phase which is where
the calcium is coming in because we get it to positive Zer and pottassium are going out so positive ions are coming in positive Gs are going out so it's kind of staying around the same membrane potential not really changing much this is phase two now we're going to stay here at phase two for a little bit because we have to see how these actual calciums are leading to contraction so now look what happens here these calcium ions until recently they kind of came up with a theory of how these calcium ions are actually triggering the
release of other calcium it's weird right calcium induced calcium releas is what they call it so what happens is these calciums that are flowing in cuz do you know they can actually flow in what is this little invagination trust me it's a word I know these positive ions these actual calcium can also flow in through this area too what is this little invagination here called that invagination is called a t tual so from these invaginations sodiums can flow into the cells and Trigger the calcium to be released here also from the actual T tubules reason
why I'm telling you this is because these calcium mines when they're coming in they're going to go to this special area with inside the cell special organel this organel is called the sarop plasmic reticulum what happens is these calciums have these special special calcium sensitive channels okay so I'm going to zoom in on one of these calciums for a second calcium comes over here and binds onto a protein one of the proteins is called calmodulin now what happens is calcium and Cal modulin or just calcium can come over here and bind on to this receptor
very sensitive receptor to calcium this receptor is called a ryanodine receptor type two so I'm just going to put R yr ryanodine receptor type two this ryanodine receptor type two which is very sensitive to calcium whenever there's increas in calcium levels this ryanodine receptor opens up a channel and when it opens up the channel guess what starts coming out calcium so now calcium is going to be really concentrated inside of the sarcoplasmic culum very very concentrated through different mechanisms but it's very very very concentrated guess what starts coming out of this area now the calciums
so now a lot of calcium is going to get released out into this actual sarcoplasm so what happened just over they're clear calcium stimulate the Radine receptor type two it can either do it directly by itself or it can combine with calmodulin and bind onto the area which opens up the Radine receptor type two which is kind of like a mechanical receptor opens up this Channel and allows for calcium ions to come out in excessively large amounts so now calcium is going to start being very high within the cytoplasm what is that calcium going to
do well calcium we're not going to spend a lot of time because we already have a video on how muscles contract if you guys haven't seen it go watch that okay we have a muscle contraction playlist right where we go over all this stuff so what happens is calcium binds onto a special protein this protein here is called troponin now this is the only one I want to spend a little bit of time on is actually consisting of of three components troponin i troponin t troponin c troponin c is where the calcium binds troponin T
is where the tropomyosin is binding to the troponin and troponin I is where the troponin is bound to actin so quickly here it's bound to actin it's bound to tropomyosin or it's bound to calcium so calcium binds onto the troponin cite which changes the shape of the troponin it binds with it pulls on troponin t troponin T pulls on that tropomyosin protein this orange protein see this orange protein right here that's tropomyosin what is it doing it's impeding the interaction between this red guy to that green guy what is that red guy there called that
red guy is called mein so this red this actual red guy here is called mein this green guy here is called actin what happens is calcium binds on jonin which changes the shape of the tropomyosin if it changes the shape of the tropomyosin what happens happens then let's actually show tropomyosin like this now so now tropomyosin is out of the way it's out of the way it's not impeding it anymore so same thing over here if calcium binds over here what's going to happen it's going to move the tropomyosin out of the way when tropomyosin
is out of the way guess what can happen the mein head can interact with the actin so calcium coming to this area increases cross Bridges cross Bridges between the Act and the me if that's the case then you're going to have more what is this kind of representing here me kind of showing the lines coming in it's representing the contraction so more cross Bridges means more contraction and then that's going to help to be able to create that pump to squeeze the blood okay so increase in the crossbridge interaction increases the contraction which is going
to cause the heart to pump action okay another thing because Gap Junctions are connecting cell to cell this is really really really really important that means that these cells are interconnected that means that these cells are basically synchronized that means that whenever these cells are receiving signals they're receiving it pretty much all at the same time very very quickly very very rapid and fast so these muscle cells that are Contracting again I could actually say that this is one muscle cell but at the same time if I were to come over here for just a
second let's say that I had over here here's another muscle cell and the ions from this one are flowing to this one or they flow over here to this one all of these muscle cells are going to be getting depolarized around the same time so they synchronize their action to where they contract as a unit they call this a functional centium not even going to attempt to spell that okay you can try to look that up or something okay how to spell it but again the whole purpose is is I want you to understand is
that these actual nodal cells are extending these Action potentials to All The myocardium through the these Gap Junctions so because of that they contract as a unit or they don't contract at all so this Contracting as a unit is actually the action of the functional centium holy crap that's a heck of a word right all right so that's that now so we've seen that action now let's get into how we actually get this cell to rest how do we get this cell to rest well we were at positive 40 molts because these voltage calcium channels
these L Type calcium channels are open when we hit positive 40 they shut off when they shut off another Channel starts opening very very very powerfully this is actually going to be called a potassium Channel and this potassium Channel opens and potassium starts exiting the cell as you start losing ton and tons and tons of pottassium ions you lose positive ions what starts happening to the inside of the cell you start losing positive ions the cell's going to start becoming a little bit more negative and it's going to become negative and more negative and more
negative and then what starts happening to the inside of the cell it's starting to repolarize so you're going to see this actual line going down on the graph you'll see it going down and it'll hit this point of resting membrane potential so now whenever the pottassium ions are coming out of the cell it's bringing the cell from positive 40 molts to around 60 MTS around the resting membrane potential but again remember these noal cells don't really have a stable resting membrane potential once they get to about -60 the potassium channels close and those funny sodium
channels start open opening so around 60 you might notice again these funny sodium channels opening and then the T type and then the L Type and then potassium repolarization okay so it's the same thing so because of that less cations are going to be coming into the cell so this cell is at its peak point now it's at that platto phase if this cell is at the plateau phase where the calcium ions are coming in and pottassium ions are going out it gets to a point where the calcium ion channels start closing so now what
happens is these L typee calcium channels start closing as these L Type calcium channels start closing less calcium ions start coming in another thing we don't want our muscles to contract forever we got to get that calcium out of there because if calcium is there it's just going to keep binding toonin and keep moving the tropomyosin out of the way so that the cross Bridges can keep moving and creating power strokes and Contracting the muscle pumping the heart but eventually the heart's going to get weak if that happens all the time we have to give
it time to rest so we got to get this calcium back into the sarcoplasmic reticulum and out into the extracellular environment to replenish the calcium levels in the outside of the cell and replenish the calcium levels inside of the sarcoplasmic reticulum how do we do that so once this happens there's going to be these special channels over you see these black channels here in the coplas reticulum these black channels on the sarcoplasmic reticulum are actually going to move some of this calcium back in so some of this calcium is going to get pumped right back
into the sarcoplasmic culum but calcium is moving against his concentration gradient because you know calcium is actually going to be in lower concentration outside the cell and in high concentration inside of the coplas critic so I'm pumping it against so that means I have to utilize ATP and usually whenever you utilize the ATP in this process you're also pumping a proton out usually so there's usually going to be an antiporter likee system where you're pumping a proton out at the same time you're pumping calcium ions in and it's utilizing ATP that's get that's replenishing the
calcium levels how else can we get calcium back in there another way that we can get calcium back in here is these calcium can actually come over to these other channels over you see these these actual red channels here these channels can actually pump some of the calcium back in also so get some of that calcium back in but again we have to have someone to help him because he's going against his concentration gradient so we found someone else and he was like Hey dude no worries I'll help you out I can move down my
concentration gradient and his name is sodium and sodium moves down his concentration gradient out of the cop plasma culum into the cycop plasm and this is an example of secondary active transport so again we got calcium back into the SR through sodium calcium exchangers or through the calcium proton ATP ases cool how do we get it back out the same channels the exact same channel so now if I take over here this black channel it's the same thing thing I'm going to take some of the calcium and pump it out into the extracellular environment so
this is the ECF the extracellular fluid this is the protons I'm going to pump it in I'm going to have to utilize ATP okay to do this process because it's primary active transport then for this one same thing I'm moving sodium down his concentration gradient and I'm moving the calcium against his concentration gradient onto the ECF that's replenishing the calcium levels back out here okay say trying to get your calcium levels out here replenished and the calcium levels in the SR replenished so now that's going to prevent the contraction so now once that happens these
calcium channels shut off calcium gets sucked back into the SR pushed out into the extracellular environment potassium channels are the primary ones that are going to be functioning now functioning now so pottassium channels are going to even open up even more and they're going to start aggressively moving out even more so as the potassium channels start even aggressively moving out even more again you're going to start losing more and more and more positive ions with no counteracting of the calcium so what do you expect if calcium is not counteracting this anymore what's going to happen
it's going to start dropping and it's going to drop and it's going to drop until it gets the resting membrane potential and then when it drops at the resting membrane potential it'll have this brief period in time where it'll actually kind of stay rested until ions from this cell let's say noal cell leak into this myocardial contractile cell again via the Gap Junctions and if that happens what happens it goes back up to threshold potential so to finish off phase two is the plateau phase so let's kind of like cut that off right there phase
one is the drop down from the potassium channels phase two is the calcium and the potassium channels phase three is just the potassium channels and then we get into this last phase which is called phase 4 and phase four is where there's just no sodium no calcium ion movement and just potassium ions kind of leaking out very very slowly to keep it at the stable resting membrane potential until the sodium ions or other cats from The Gap Junctions leak into the cell again and triggered to go to threshold holy crap okay that's that now with
that said we see exactly how this muscle is communicating that's the intrinsic ability all right Niners if you guys have stuck in there throughout this entire video here where we talk about electrophysiology and very great detail um I want to thank you guys enough we're going to I can't thank you guys enough but we're going to go into part two so we talked about the intrinsic ability of the heart what I want to do now is I want to get into a little bit more of the detail of the extrinsic interation of the heart how
that can actually uh bring the actual Baseline of the intrinsic ability of the heart above the actual like you know basically increase in the heart rate or how we can bring it below that actual basil rate which is going to be decrease in the heart rate which is called bradicardia increase in the heart rate Tac cardia so we'll talk about how the sympathetic and parasympathetic nervous system affects this activity so I hope to see you guys in part two all right see you soon n nerds
Related Videos

20:33
Cardiovascular | Electrophysiology | Extri...
Ninja Nerd
551,540 views

21:55
Cardiovascular | Structures and Layers of ...
Ninja Nerd
1,139,728 views

1:19:14
EKG Basics | How to Read & Interpret EKGs:...
Ninja Nerd
2,699,328 views

3:11:52
Diagnosis of SVT in the EP lab
Dr. Joshua Cooper - Arrhythmia Education
114,633 views
30:01
The Cardiac Action Potential
Strong Medicine
52,065 views
40:20
Cardiovascular | Fundamentals of Blood Pre...
Ninja Nerd
1,018,738 views

2:52:11
Drugs for Heart Failure
Ninja Nerd
351,038 views

23:59
Cardiovascular | Cardiac Cycle
Ninja Nerd
1,636,870 views

58:46
Understanding Electrophysiology Lab Concep...
The Texas Heart Institute
11,185 views
42:02
Cardiovascular | Blood Pressure Regulation...
Ninja Nerd
699,879 views

45:43
Musculoskeletal System | Smooth Muscle
Ninja Nerd
406,606 views

17:46
Heart Conduction System & ECG (EKG)
Siebert Science
123,139 views

59:14
MASTER ECG/EKG INTERPRETATION: A Systemati...
Ninja Nerd
1,943,452 views

26:12
How to Remember Everything You Read
Justin Sung
2,056,657 views

56:30
Neurology | Resting Membrane, Graded, Acti...
Ninja Nerd
1,384,393 views

23:27
Cardiovascular System 3, Heart, electrical...
Dr. John Campbell
760,869 views

44:59
Cardiovascular | Cardiac Output
Ninja Nerd
1,311,589 views

18:31
Understanding Arrhythmias
Zero To Finals
115,063 views

25:40
Living With A Pacemaker (common questions ...
Dr. Joshua Cooper - Arrhythmia Education
43,720 views

19:26
Cardiovascular | Blood Vessel Characteristics
Ninja Nerd
369,298 views