Arrhythmias | Clinical Medicine
180.91k views12017 WordsCopy TextShare

Ninja Nerd
Exclusive USMLE Step 2/PANCE Lecture… for FREE! Become a member on our website for more Premium Reso...
Video Transcript:
[Music] H what's up Ninja nerds in this video today we are going to be talking about a monster of elure we're going to be talking about arhythmia and there's going to be a lot of stuff to go over so let's get right into it guys so first things first we're going to talk about two different types of arhythmia one is when you're going just too slow this is called your Brady arhythmia and then we'll talk about another one you're going way too fast and this is often referred to as your tacki Aras so when we
talk about Brady Arias I think one of the biggest things to be able to remember here is that we're going to talk about this in two different blocks one is we're going to talk about sinus bradicardia and the other one is we're going to talk about AV blocks but we'll get into the different types of Av blocks more when we get into the diagnostic section so first things first sinus braic cardio versus AV blocks how do they differ pathophysiologically when we talk about sinus braic cardio this one is usually due to a dysfunction of the
a SA node so the SA node is just not sending the action potentials approach appropriately at a good enough rate from the SC node through the Atri to the AV node so therefore the AV node is not receiving the electrical activity appropriately and it's not conducting that down into the ventricles to generate an appropriate ventricular rate so therefore it's decrease conduction decrease conduction and therefore the ventricular rate will be low usually less than 50 now often times Brad cardia most textbooks will say it's usually less than 60 I personally like to go to like less
than 50 beats per minute for truly concerning bra cardia all right I think the thing to remember though is like what is driving the sinus node dysfunction the SA node dysfunction there's a bunch of different things so one of them I really would want you guys to think about is noal blockers the common one is beta blockers especially if it's an beta blocker overdose so in patients are taking maybe too much mopal law Carval law Lial law these have the capability of blocking the beta 1 receptors in other words norepinephrine epinephrine can't bind to these
receptors therefore they can't cause calcium influx therefore this cell does not actually depolarize and send action potential that's what leads to the SEO dysfunction the big thing to remember with beta blocker overdose is that usually it can be reversed by giving the patient the antidote such as glucagon what's another one calcium Chanel blockers are another drug this is usually Verapamil deltm this is commonly given to patients who like have atal fibrillation or some type of underlying Tachi rhythmia if you give them too much of them they block the calcium channels calcium can't run in if
calcium can't go in they can't depolarize they can't conduct electrical activity from the SC downwards that leads to the actual bra cardia now the antidote that would lead to the reversal of the braic cardio would be calcium and so it's important to remember that the next one's dexin dexin is often given to patients who have atrial fibrillation um it can also be given to patients who have heart failure with a reduced ejection fraction less than 35% this one's weird it has two functions one is is it has a a negative chronotropic action and a positive
inotropic action we'll talk about that one a little bit in the tach rhythmus but with noal blockade how this one works is it increases the acetylcholine in the synapsis and has them activate the muscarinic 2 receptors when you activate muscarinic 2 receptors that causes a potassium iion e flux that hyperpolarizes the cell makes it negative therefore it will not conduct electrical activity and lead to a decreased heart rate often times with the Jox and toxicity the big thing to remember is giving these patients Digi bind will often lead to the reversal of their braic cardia
another one that I person like to consider as a nodal blockade is hyperkalemia especially when the potassium starts reaching six or seven I see a couple things one is I see PT waves I also may see a prolong PR interval and that's where you might start seeing the brto cardio but I also kind of see like wide qrs's they can go into a sine wave pattern and even break down into like viib PA arest is very common as well the concept behind this is that they inactivate the sodium channels it's actually very interesting so if
you can't bring sodium into the cell you can't depolarize it you can't send action potentials from the essay node and this is also problematic for the AV note but we'll get into that how it does it do this though it does it by actually increasing the resting membrane potential now watch this here we have a normal graph right so here's going to be this part here's going to be this part so time and voltage so here's our normal resting memory potential whenever the potassium's too high outside the cell potassium inside the cell can't leave so
it stays in the cell and therefore the resting membrane potential starts Rising there's the new one now you would think okay I start from a resting M potential I depolarize then I repolarize and I would go back down to this point here at this black dotted line that's where the sodium channels go from the inactive State into the resting state and ready to be reactivated again but if you have a new resting membrane potential via the Blue Line they'll never make it to the state where they can actually become reactivated again they can be ready
to be activated again so they'll never reach this point so they'll always stay inactive and that's what leads to this process one of the big things if you start seeing Peak T waves prolong PR interval um maybe a wide Qs complex s wave pattern give them calcium it stabilizes the cardiac membranes and that's the big thing to remember for this one now these are common things that you can actually elucidate a lot from just their medication history or even talk to them about potential diseases they have and do they take any medications for their underlying
diseases another big thing is high vagal tone so when a patient has neurological catastrophes subid hemorrage I maybe they have like some type of traumatic brain injury and their intcal pressure shoots up what it may do is it may trigger a reflex activity of their vagus nerve the vagus nerve when it actually acts on the heart it releases acetylcholine this sounds familiar acetyl cooline acts on the MUSC two receptors just like de join that causes potassium anux hyperpolarizes the cell can't conduct electrical activity and therefore if it can't it can send the action potentials from
the acde fast enough you got to then think does the patient have any neurological deficits in combination with the Cushing Triad which is braic cardia hypertension and irregular breathing another one is decreased sympathetic tone this is usually in the form of a severe form of hypothyroidism often known as mixoma in hypothyroidism the beta 1 receptors are less sensitive norrine epinephrine therefore whenever they bind they don't exibit the actual same effect and what they're supposed to do is bind to the beta 1 receptors and cause calcium influx if they're not sensitive to the norepinephrine epinephrine they
won't cause calcium influx they won't depolarize and they won't send action potentials all of these things that we just talked about is the driving factor of sinus bra cardia what about the next concept here and Pati to of hypothyroidism one quick fact before we move on is that often times if it's mixed deacom they'll have hypothermia their temperature will be very very low they even have features of like integumentary dysfunction so miedema usually on the pretibial region and sometimes even on the periorbital region the last thing is just check their thyroid function test that also
may be indicative especially if the T3 T4 level is low and you can check their TSH to see if it's you know primary or secondary all right we move into AV block so here's the interesting thing with AV node block the problem with this one is that the SA node is firing but the AV node is not receiving it and conducting the electrical activity down into the ventricles that's that's the problem here here so if the AV node is not conducting the electrical activity that's what's going to lead to the ventricular rate being low where
the heart rate's less than 50 here's the concept which is very nice and saves us a lot of time what causes the AV node dysfunction everything we just talked about for the SA node dysfunction so think about beta blocker overdose calcium channel blocker overdose dexin overdose hyper calmia uh low sympathetic tone like hypothyroidism especially mixoma and neurologic catastrophes like Cushing syndrome all right Cushing's Triad I apologize all right the last thing to think about for AV node block besides what we thought talked about for SE node dysfunctions for sinus pric cardio is nodal destruction so
if you destroy the AV node that thing ain't going to work it's not going to conduct Electro activity so what are some reasons for this one another one would be an inferior Mi so you know you include the right corner artery that's supposed to supply the right ventricle and so for these patients if you knock out their right coronary artery they'll have an infarction of their right ventricle but also their AV node if you infar their AV node that thing's not going to work it's not going to be able to send action potentials and that's
going to lead to to this problem here it's not going to be able to conduct the electrical activity if it's destroyed another one would be lime's disease you know lime carditis whenever you have a really bad infection here where they produce a bullseye rash right this one can also infect the AV node and it could potentially lead to a third degree AV block and the last one be old age this is usually due to cile fibrosis so cile cardio fibrosis of the ab node is very very common how do I differentiate these in inferium they're
going to have angena right they're probably going to have some tronin elevations and get an EKG look for STS elevation and 23 avf and line look for that Bullseye rash in combination with the third degree of block often times they'll respond to what sep aone usually limes you treat with doxycyclin but if they have limes carditis you give them seaon all right that's our Brady arhythmia not too bad right all right my friends now we're going to move on to the pathopysiology of Tachi rhythmus now there is many different types of these let's talk about
the super ventricular ones so what are they sinus Tac cardia multifocal atrial tacac cardia proyal super ventricular tacac cardia often times you may just heard this as SVT another one would be atrial flutter atrial fibrillation these are your super ventricular tthms meaning that they originate usually above the AV node all right so there's going to be some type of process that's involving the Atria where these AR Ares are originating if they originate from the ventricles then it's referred to as ventricular tardia or ventricular fibrillation or torsades dep points now regardless of which type of arhythmia
this is Tachi arhythmia it's important to remember what's driving these and there's three pathophysiological Concepts that are responsible for this one is enhanced automaticity now what this generally means is this can be thought of in two ways one is it's enhanced normal automaticity which means that your SE node is firing to your AV node to your bundle of His to your bundle branches to your bingi system way faster than normal or it's enhanced abnormal automaticity you have an area in the Atria that besides the SE node that's firing sending information to the AV node to
the bundle of His to the bundle branches and it's moving very fast you just have to ask yourself the question is what's causing this increased activity through the conduction system and usually it's increased sympathetic tone how does this do it well increased sympathetic tone means that you're going to stimulate the beta one receptors pretty heavily in The myocardium the reason why this is important is because the sympathetic nervous systems usually when it's increased in activity it's causing a lot of norepinephrine epinephrine release this hits the beta 1 receptors this causes calcium influx that depolarizes the
cell that causes increased conduction through this system and that's where the increase in heart rate comes from because if I have increased as a node conduction or increased conduction through the AV node my ventricular rates are going to be super high greater than at least 100 beats per minute that's the concept with increase automaticity so what we'll do is later we'll talk about what are the things that increase sympathetic tone all right another thing that can drive arym is is what's called re-entrance circuits so this can to occur in the Atria so here you see
this circus movement around this particular area within the Atria as it moves through this kind of like area in this circus pattern as it does that it sends off these electrical activities that kind of move down through the AV node bundle of hiss bundle branches and this can lead to some pretty nasty High rates right the concept here is what's causing the circus movement usually it's atrial or modeling that causes heterogeneity so changes in the actual tissue makeup and usually the atrial modeling is due to a lot of pressure or volume inside of the Atria
that's stretching out the Atria that causes this heterogeneity so then you have to ask yourself the question what's causing the stretching and that's usually CHF right that's a definite one another one would be hypertension or mitosis right the valvular heart disease another concept what if it's in The ventricle what if there's this area where there's a lot of circus movement moving around here and it's sending off a lot of these electrical activities here right this would be the same thing all right well this is usually due to ventricular Remodeling and usually that's a fibrotic scar
due to ventricular f fibrosis what can cause a scar a myocardial infarction what could cause stretching CHF usually systolic heart failure so in other words you have to have CHF with a reduced ejection faction less than 35% that's pretty bad or you have to have a very bad myocardial infarction that occurred there these are drivers of re-entrance circuits because they create heterogeneity within the myocardial tissue and create this circus movement and as you create this circus movement you send off these electrical signals every time you run through that and that's dangerous all right the next
concept here is going to be triggered activity now with increased triggered activity what is this concept how does this work well let's say here you again you're normally supposed to have movement going from the SA node to the AV node to the bundle of hiss and the bundle branches what if I have an area besides the SA node that's firing at a very very fast rate and it's kind of driving this activity down this is called ectopy right so there's an ectopic focus and it's in the Atria this whenever it fires if it fires at
a fast enough rate it can cause tacac cardia the other one would what if it occurs in The ventricle well then this is a ventricular ectopic focus and this can definitely fire at very fast rates as well so you can see Taco cardio with this the question is is what's causing this little ectopic area to start firing undesirably well usually it's due to depolarizations that come you know before the the actual Hearts had the complete time to repolarize and rest and we call these after depolarization so there's two types one is early after so in
other words you have here the UPS sloping so this is the depolarization phase then you got the plateau phase and you're starting to go into the repolarization phase what happens is before this thing can completely repolarize you just stimulate it and cause it to start firing so what would do that a lot of different things but again it has to occur early usually this is due to something that kind of prolongs depolarization like prolongation of the QT interval this is there's a couple different things hypokalemia hypomagnesemia a bunch of different drugs we'll go over that
though but this is the big thing here that's the primary reason for Eads early after depolarization the other one's dad so it's delayed after so again here's your polarization here's your Plateau phase here's your repolarization it's going to occur later so it's delayed so as it's getting ready to repolarize Boom you stimulate it and it starts firing this is usually going to be due to a lot of calcium influx into the cells and that's the primary driver for the dads the delayed after theorization this is a lot of sympathetic problems myocardial infarctions deox and toxicity
which again we'll talk about a little bit later but these are the three mechanism my friends three mechanisms that drive often times different tormas so now what we got to do is we got to go through each type of tacki rymy and talk about what are which maybe which one of those pathophysiological processes occur and what drives that pathophysiological process all right here we go sinus tactic cardia is primarily driven by increased automaticity so increased sympathetic tone so then you have to ask yourself the question why is the SA node firing faster okay the sympathetic
activity is high why is the sympathetic activity high is the blood pressure low why would that be a cause you know when your blood pressure drops right it activates the be receptors and your CDs and your aorta tells your actual brain brain stem especially the cardiac exelator center hey send a lot of sympathetic outflow that sympathetic outflow leads to a lot of norepinephrine epinephrine release especially onto the my cardium hits the beta 1 receptors and shuttles a lot of calcium and sodium into these cells which depolarizes them and increases the conduction from the SA node
to the AV node downwards increasing the heart rate so you have to think about is the patient's blood pressure low and if it is low think about causes are they in cardiogenic shock are they in obstructive shock are they in septic shock hypmic shock work them up for that increase their blood pressure and their tach cardia should improve are they hypoxemic is their pao2 less than 60 mm of mercury do they have a low O2 saturation if they are it could be activating the chemo receptors the peripheral chemo receptors and the katees and the aorta
activating the sympathetic nervous system trying to increase your uh heart rate to increase your cardiac output why because if you increase your cardiac output that'll increase your blood pressure If you increase your cardiac output you push more blood to the lungs which will help with gas exchange to improve your VQ matching that's the concept here but think about causes often times you know the most common cause is pulmonary embolism maybe even pneumonia or severe COPD exacerbation another one that's actually really weird because it can be it can cause like an anemic type of hypoxemia severe
anemia so think about that one as well hyperthyroidism is interesting because what happens is especially if a patient has what's called thyroid storm and thyroid storm remember hypothyroidism decrease the sensitivity of the beta 1 receptors hyper thyroidism increase the sensitivity of them so now you have a lot of calcium influx sodium influx a lot of depolarization you know what else hyper thyroidism does it also increases your metabolic rate if you increase metabolic rate of cells they're going to fire and move a little bit more like faster you know what else increases your metabolic rate fevers
which can be due to a lot of different things especially hyperthyroidism and when you increase metabolic rate that naturally directly can increase the activity of these myocardial cells and cause them to fire faster it's important to remember for hyperthyroidism think about them having an increased body temperature in combination with evidence of hyperthyroid levels and I think it's important to remember that you can actually treat these patients with propanolol and that oftentimes May improve their underlying tacac cardia with fever you just treat their underlying cause of the fever or give them Tylenol cool them and often
times that will improve their underlying tacac cardia other reasons why patients can be tacac cardic is what could be some pathomimetic drugs so drugs that act like norepinephrine epinepherine so they exhibit the same beta 1 stimulation think about a patient who has maybe asthma COPD exacerbation getting tons and tons of Albuterol that could cause this or they're hypotensive and they're on norepinephrine epinephrine those stimulate the beta 1 receptors and can increase your blood pressure and your heart rate on top of that cocaine methamphetamine if these patients are exhibiting types of activities that are concerning for
drug use check a talkx screen to see if those are coming back positive and lastly if a patient has like palpitations headaches diaphoresis hypoglycemia hypertension tacac cardia that are intermittent work them up for Via chromosom if you have a high degree of Suspicion by checking some urine and SE metan nephrin these are the most common reasons why patients can develop pyoc cardia besides I wouldn't forget pain and anxiety pain and anxiety can also lead to very common increased sympathetic tone all right that's the big thing to remember for this one multifocal atrial tacac cardia yes
can also be due to increased automaticity but the primary reason why this one develops is not all of these things that I talked about it's one thing it's often times chronic hypoxemia the big thing I want you to remember and write down guys is the COPD in patients who have COPD or they use the drug that we use to treat COPD like theophine this is often times the most common cause of multifocal atrial tacco cardia another one's called proxis Mal super ventricular tardia this one's due to re-entry all right now you're like oh that's that
like the weird circus movement that occurs in different areas and causes the electro activity to get sent down into the ventricles or maybe it originates from the ventricles either way I know that it's a circus movement my question is is why is this circus movement developing well I know that if if it was like the Atria the ventricular ones it was like stretching right of the Atria or remodeling of the Atria remodeling of the ventricles what if it happens just because it was already there what if it's anatomical it has nothing that to do with
any underlying disease processes or remodeling per se this is when I want to talk about this guy so there's two different types of psvt if you will one's called avnrt so AV noal reentrant tacac cardio so there's some type of re-entrant circuit that's kind of originating here in the AV no so if you zoom in on it imagine here's kind of an electrical conduit coming from the Atria to the AV node here and what happens is there's like this little fibrosis that occurs here in these patients and it creates these two Pathways one will depolarize
very very slowly and the other one will depolarize super fast and because of that it creates this heterogeneity which leads to this weird circus movement and so what happens is electrical activities will then kind of create this movement which causes every single time it goes through this cycle to spit off electrical activity down to the ventricles super fast the concept behind why this happens why you'll have this circus movement is because the heterogeneity causes a slow pathway so this pathway can you know usually depolarize very slowly but repolarize very quickly and then this pathway depolarizes
really really fast but then repolarizes really quickly so it creates the perfect opportunity for a circuit to continue to move through this in the most perfect Manner and it can create very very dangerously quick arrhythmias or tacac cardia I think one big thing to remember for this one is often times you won't be able to really see a p-wave sometimes the actual p waves may be there but they're often times maybe like retrograde p waves that I would be potentially looking for another anatomical one is called wolf Parkinson's white syndrome it's an AV re-entrance Tac
cardia and it's usually due to the thing here called the bundle of Kent it's like this like entryway between the Atria and the ventricles and so it allows Action potentials to travel directly from the Atria into the ventricles now the danger of this is that this can bypass the AV node so imagine if a patient had atrial fibrillation and they're beating at a rate of like 200 250 if they go through the bundle of Kent because they bypass the AV node then the atrial rate can equal the matricular rate patient can go into vfib easily
and so that's terrifying to remember if the patient doesn't have a pre-excitation syndrome like apib though often times the classic things that we look for in the ECG for Wolf Parkinson's white syndrome is the Triad known as a decreased PR interval a wide QRS complex and a Delta wave and this is something that we'll talk about a little bit more in the ECG interpretation all right atrial flood or atrial fibrillation this one's interesting so increased automaticity can drive this process the problem is is that usually it's not the the primary thing that causes a patient
to go in atrial flutter and atrial filation it can be a trigger though so for example let's say that a patient's hypotensive or hypoxemic hyperthyroid or they're having fevers or they're taking a sympathic drug that's going to increase the automaticity it's going to cause these areas to want to fire faster but then combine that with a re-entrance circuit and that's where you start seeing patients who start developing some pretty nasty atrial fibrillation and atrial flutter so atrial flutter usually has this reentrance circuit called the cavotricuspid ismus and that's a really large reention circuit here so
if a patient has this and then on top of that they become hypotensive hypoxemic hyperthyroid um they take some sympath Medics or they have a really bad fever this can put them into a very bad atrial flutter same concept if a patient has atrial fibrillation they usually have these like reentrance circuits that occur in multiple areas but usually right around the entry of the pulmonary veins so if you have these and then on top on top of that the patient becomes hypotensive hypoxemic hyperthyroid fibral takes a sympathetic drug boom you can pop them into atro
fibrillation here's another concept if a patient has those re-entrant circuits they have high sympathetic tone and then on top of that you add in some triggered activity some increased early after depolarizations and you cause these ectopic fosa to fire more abnormally what could D try drive this hypokalemia hypomagnesemia all of these things can prolong the QT interval prolong depolarization and push them to have these Eads the triggered activity so what I really want you to remember is Atri flutter and Atri fibrillation is a combination of all of these it's usually a patient has a re-entrance
circuit so they have for example Atri fibrillation to have those reentrance circuits due to atrial modeling so they had underlying hypertension they have CHF they have mitro valve stenosis that's causing the reenter circuits by increasing the left atrial pressure and atrial modeling that's their chronic problem then you add a sympathetic tone you make them hypotensive you make them hypoxemic you give them hyperthyroidism you give them a drug or you give them a fever or you make them hypemic hypomagnesemic that's enough to drive them into that disease process that's the thing I want you to remember
now with that being said ventricular tardio ventricular fibrillation same concept it's usually not just this that puts them into ventricular Tac card it's a combination of things so for example if a patient goes into vtac or viib they may have one of these potential factors going on in combination to having a re-entrance circuit so in other words they have to have some ventricular remodeling that must be going on remember here that this could be due to in ventricular is Circus movements due to a fibrosis so maybe they had a myocardial infarction right or maybe they
have heart failure with a reduced ejection fraction less than 35% and that's causing this area here to become super act agitated and create re-entrance circus due to the heterogenity in the pathways again I think one quick thing to remember here is that there's two different types of ventricular Tac cardio one is if you only have one of these guys here it's called monomorphic all the Qs complexes look the exact same or you could have like maybe more than one so two or three of these potential areas then it's going to cause all the Qs complexes
to look a little bit different because they're coming from different areas in the ventricles and that's called polymorphic but either way in ventricular Taco cardio you need a re-entrant circuit usually in combination with increased sympathetic tone another one of these is ventricular fibrillation you need to have these particular areas multiple areas of re-entrance circuits in combination with having a patient have increased sympathetic tone so usually a patient has an MI they have heart failure and then on top of that you make them hypotensive hypoxemic you have them hyperthyroid fibros sympathic drug boom puts them into
vtac or vfit what makes it even worse is that triggered activity can also propagate this process again it's multiple things so are they hypoc IC hypomagnesemic that can also cause them to develop vtac and viib especially in combination with a re-entrance circuit and increased sympathetic tone now with triggered activity there is Eads but there was another one what was the other one dads so with dads this is usually due to increased sympathetic tone that can massively increase calcium influx by increasing the beta 1 receptor activity you know what else myocardial infarction this is a really
big one so myocardial infarction can cause both triggered activity and re-entry the concept by myocardial farction is usually the patient will present with anguna they'll present with an elevated troponin they'll present with SD changes and then on top of that you know what's really important for this one when you infar a tissue cell you lose the entire like cell Integrity so it's not as you know semi-permeable as it used to be so calcium can just easily influx into these cells and that's one of the problems here is why they get a lot of calcium influx
because dads is calcium influx Eads is prolonged QT what's another thing that can actually cause calcium influx deox and toxicity it's really weird because usually this one will it'll respond to digine but the concept here is that with the Jox and toxicity inhibits the sodium pottassium atpases in these myocardial cells and if you do that you prevent sodium kind of you inhibit the actual sodium exchange and so the sodium inside of the cells is much lower the problem with that is that now I can't properly exchange the calcium and so calcium kind of builds up
inside of these cells and as a result calcium levels really high in the cells depolarizes the cells and causes them to develop triggered activity so the big thing that I need you to remember here my friends is that ventricular Tac of cardiio ventricular fibrillation atrial flood or atrial fibrillation they all often depend on a combination of all three of these things to put a patient into these deadly arrhythmias the last kind of tacki Rhythm here is torsa points this one's really only dependent upon triggered activity and so usually this patient has has some type of
hypokalemia hypomagnesemia that's prolonging their QT interval but then what you do is you throw in some drugs that also prolong the QT interval even more and what happens is it's so severe that this can actually cause a patient to go into torsades so have hypokalemia and hypomagnesemia plus QT prolonging medication recipe for disaster so what are some of these drugs I like to remember the anti rythmics such as amum abuy is a common one antibiotic like macrolides antis psychotics which helps with the pneumonic here such as haloperidol another one would be anti-depressants ssris tcas and
anti Medics like honron or Compazine either way if you have any of these medications in high doses in combination with hypokalemia hypomagnesemia it's enough to prolong the QT interval prolong the depolarization and shoot them into this triggered activity which can cause tors Oda points so I know that this is a lot to remember I just want you guys to try to to be able to understand that again all of these arrhythmias are dependent sometimes on multiple different concepts it's not just one pathophysiological process that leads us to The Next Step patients who have arhythmia sometimes
they can be completely like asymptomatic it's more like an incidental finding sometimes it can be super terrifying but what I really want you to remember here with arhythmia is how do I how to identify an unstable arhythmia versus a stable arhythmia so in patients with unstable arhythmia often often times there's the Brady and the tacky the bradies often times we'll talk about these we haven't gotten to them yet but second degree mobit 2 and third degree AV block are usually the most severe Brady arhythmia you can see you know un instability with sinus bradicardia first
degree second degree mov it's one but it's not going to be as common these are really really bad and these would directly drop your heart rate and we'll talk a little bit about how that can cause instability in a second with respect to tack rith means there's a bunch of them right atrial fibrillation atrial flutter proxis Sy super ventricular tacac cardia ventricular tacac cardia all of these can kind of generate some pretty fast heart rates and your heart rates can go up to greater than 150 now how do these cause instability per se well let's
start here with this one because this one's really easy with an increased heart rate your diastolic time frame is reduced significantly you don't allow for the ventricles to be filled appropriately if your ventricular filling is reduced what happens to your preload your preload drops if your preload drops what happens to your stroke volume that drops if your stroke volume dropped what happens to your cardiac output it drops before we move on to the next step what's the cardiac output equal to heart rate times stroke volume if heart rate drops that's going to do what drop
the cardiac output here's the interesting concept with severe braid cardia it'll directly drop the cardiac output with severe tacac cardia it in directly drops the cardiac output by dropping the ventricular filling now when cardiac output drops that drops your blood pressure because blood pressure is equal to cardiac output times your systemic vascular resistance so if blood pressure goes down I'm not going to peruse organs like the brain and so they can syncopize they can develop confusion they can have declining level of Consciousness such as maybe lethargy maybe they can become super fatigued obtunded and this
is very important to remember because this is what I refer to as an altered mental status if they're not profusing their myocardium so they're not getting enough blood flow out of their left ventricle to fill their coronary arteries are they going to give enough oxygen to their coronary uh to their myocardium no if The myocardium becomes aeic what is the most common presentation of myocardial lemia angena so if a patient has alter mental status and angena that's an indication of instability regardless of their super bra cardic or tacac cardic if their cardiac output from their
left ventricle is low enough that they're not getting blood out of their left ventricle into the order it can backflow into the pulmonary veins into the actual alvioli and cause pulmonary edema pulmonary Reda often times presents with severe dnia and sometimes hypoxia if that happens that's an indication of acute heart failure and again that is an indication of instability in the context of Brady arhythmia or tach arhythmia the last one is is the patient's blood pressure enough that it's really really low way below our normal limits so there's there's two different definitions here there's hypotension
and then there's shock hypotension we often Define as a couple different ways systolic blood pressure less than 90 a diastolic blood pressure less than 60 but I prefer the next one here which is a map a mean arterial pressure less than 65 because that's our profusion pressure if these are low then the patient is considered to be hypotensive and that's enough so if a patient's tartic bra cardic and hypotensive that's enough to consider them to be unstable take it a step further they're hypotensive and you have to add on drugs to push their blood pressure
up such as inotropes to make their heart squeeze more or Vaso pressors to squeeze their blood vessels because if you squeeze blood squeeze the blood vessels your resistance goes up and if res what is blood pressure equal to cic Output times resistance so resistance goes up blood pressure goes up if you're using these drugs to try to maintain a good blood pressure you're in shock and that's a concerning finding another thing that concerns me of shock is if they're hypotensive on these medications plus their lactates elevated because it means I'm not profusing my organs appropriately
and then even worse than that if I have a High lactate hypotension requiring pressors and I'm having to compensate and squeeze my vessels and basal constrictum that my extremities are becoming cold pale model that means my resistance is way too high and I'm in a shock state if I have hypotension if I have alter mental status angena hypoxia ornia or worst case scenario full-blown cardiogenic shock that's an indicator of instability in that setting of an arhythmia okay okay the next complication the most terrifying is cardiac arrest and this can be seen in four different types
but we'll go through this in the sense that the patient is an abnormal electrical activity they're not generating a good enough cardiac output and actually I would say they're not generating a cardiac output at all therefore if they're not getting blood out of their heart into their actual circulation they're not generating a blood pressure if you're not generating a blood pressure if I go to feel the radial pulse I won't feel one so they don't have a pulse therefore they're not profusing organs if they're not profusing organs are now considering this patient to be in
Cardiac Arrest the type of cardiac arrest that they are in depends upon the type of Rhythm that they're in so are they in PA arrest meaning that they have an organized Rhythm on their ECG so it looks like normal sinus but they don't have a pulse that's paa do they have a flat line in the no pulse that's asy these are nonshockable rhythms in other words you don't defibrillate these patients you just do compressions and give them Epi in the other scenario do they have vtac do they have a wide and um a wide type
of regular tacac cardia that's concerning for ventricular tacac cardia and that right there is a shockable rhythm and then lastly do they have this wide irregular Rhythm that's consistent with viib that's also shockable Rhythm so these are shockable this is not shockable the question that you have to ask for these patients is what drove their Cardiac Arrest why did they go from having an arhythmia to having pretty much no blood pressure no pulse and you want to remember these based upon the ease of them especially during a code which is the H's and T's so
as a patient is undergoing the CPR process you want to be evaluating the underlying cause could it be due to hypoxia could it be due to hypotension that they're having this could it be due to severe acidosis could it be due to hypo or hyperkalemia that's causing this could it be due to hypothermia could it be due to tanod which is causing an obstructive shock tension numor causing an obstructive shock is it a thr particularly within the myocardial kind of area the coronary vessel so an MI causing cardiogenic shock is it a PE causing obstructive
shock and severe hypoxemia or is it toxins that are driving this process the reason why it's important to know this is that if you kind of treat these you may prevent them from either going back into cardiac arrest or take them out of cardiac arrest give them oxygen increase their blood pressure maybe give them volume give them basal pressors give them bicarb give them potassium give them calcium and get rid of the excess pottassium warm them up do a paric cardiio synthesis do a chest tube give them TPA give them TPA reverse the toxin if
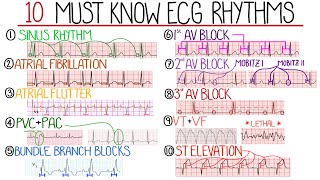
possible that's the concept and why this is important all right my friends now let's talk about the diagnostic approach to bradio rhythmus so for these patients if they're coming in they're braad cardic heart rate less than 60 preferably ey like less than 50 then you first need to do the first thing you need to do is obtain an ECG the reason why this is going to tell you if it's a sinus braic cardio or an AV block and then we're going to go through the different types of Av blocks I I'm excited to show you
guys this so first things first when you look at the ECG you have to ask three questions is there a sinus rhythm in other words if I look at this ECG here is the p-wave upright and lead to an inverted in AVR if it is that's kind of indicative at least sinus rhythm next thing if I look at these and I go after the Rhythm strip and I look at every single component after every p-wave is there a Qs complex if there is okay it's still potentially sinus pric cardia the last thing I have to
have to make it sinus predic cardia is I have to have a normal PR interval meaning that the distance from the beginning from before right before the def upward deflection to the point where I have my downward deflection for the Q wave of the QRS complex I have to have this between 160 to 200 milliseconds which is usually less than one big box if that is the case it's normal then this patient has sinus braic cardia if they don't meet these definition in other words I drop a QRS complex somewhere my PR intervals abnormal it's
an AV block and then I have to just decide what type of Av block I have so how do I do that I like to look at these and kind of go through this so the first one is is the PR interval prolong meaning it's greater than one big box so if I zoom in on it is this greater than one big box and it 100% is it's greater than 200 milliseconds so therefore I have an AV block I just have to ask myself the question in order for it to be a first deegree you
can't drop a QRS it's just a prolong PR interval do I drop any qrs's here no that's a first degree is my PR interval getting when I zoom in here longer and longer and longer and then do I drop a QRS complex because if I do that's a second degree moit one so it's longer longer drop you have a winky boock right the next thing is if I zoom in here on my rhythm strip is the PR interval constant but then I just randomly drop a QRS complex here after that p-wave if that's the case
that's a second degree mobitz 2o and then lastly is if just like I look at this thing and there's like a ton of p waves and then there's a you know a bunch of curus complexes that are usually maybe wide meaning it's an infranodal block or I just see a bunch of p-waves and they're beating at their own rate and there's just really no relationship between the p waves and the QRS complexes this is complete atrial ventricular disassociation this is 100% a third degree a block so now that takes me to the next one which
is diagnostic approach to tach your rhythmus so now again patients greater than 100 beats per minute next thing I have to ask myself is okay get an ECG look at the ECG and look to see what the actual QRS complexes look like do they look wide or narrow if it's narrow if I were to measure between this Qs complex it has to be less than 120 milliseconds that's three little boxes if it is then it's a narrow Tac cardia then I ask myself the next question what's the intervals is it regular irregular so then I
have to look at the r to R interval so if I look here and I measure the distance between each R to R interval if they're the exactly the same all the way down this Rhythm strip here that's a narrow regular Tac cardia and I have three differentials one is sinus Tac cardia psvt and two to one atrial flutter all right let's go through each one of these with sinus saic cardia oftentimes if you zoom in on the lead two it's upright and lead to right and it's inverted p-wave in AVR and then every p
wve is followed by Q complex that's sinus tacac cardia so again upright and Lead 2 inverted AVR every pwa followed by cures complex and their tacac cardic at sinus tacac cardia if I look here and I see no p waves then I'm saying okay this could be psvt oftentimes it can be difficult if they're going super fast and I like to do a vagel maneuver or Denine and it stretches them out a little bit more but in this particular scenario for psvt you're looking either for no p waves or potentially some retrograde p waves all
right the next one's atrial flutter atrial flutter I like to look in two three avf sometimes even flip the ECG upside down and you're looking for these like flutter waves which is usually pretty common and indicative of 2:1 atrial flutter now when I see these and I say oh it's sinus Tac of cardia then I got to go back and think what was the causes oh okay well it was you know maybe low blood pressure hypoxemia maybe it was hypothyroidism maybe it was a fever Sy paatha Medics treat those things and see if they get
better if it was psvt it's usually some type of like abnormal re-entrance circuit that's usually due to an anatomical problem often times there's nothing that's usually driving this it's just this abnormal anatomical process and then for atrial flutter it's usually a re-entrance circuit the cable tricuspid dismus in combination with trigered activity hypomagnesemia hypokalemia or increased sympathetic tone hypotension hypoxemia hyperthyroidism sympath Medics and and then fevers so again treat those and see if the patient can get a little bit better the next thing is if they have a again a narrow QRS and a abnormal R
to interval meaning that when I measure these they are not the same throughout then this patient has a narrow irregular tacac cardia and this gives me pretty much two differentials atrial fibrillation I like to look in V1 really for atrial fibrillation and what would help me is that I'd be able to see like these fibrillatory waves that would usually be indicative of atrial fibrillation the other one is multifocal atrial tacac cardia kind of try to zoom in on the Rhythm strip here and I would try to look for three morphologically different p waves and if
I can see that that's super indicative of multifocal atrial tachicardia now with that being said atrial fibrillation is a re-enter in circuits due near the P entry of the pulmonary veins Plus hypocam hypomagnesemia or increased sympathetic tone hypotension hypoxemia hyperthyroidism some type of sympathetic drugs as well as maybe even fever treat those and see if it can fix the patient's underlying cause multifocal atactic cardia usually COPD or theop in use now we go to the opposite side so we go down the other arm so now the Qs complex is greater than 120 milliseconds that's why
it's greater than three little boxes and why attack of cardia look at the RR interval is it normal in other words if I track all these out is it going to be the same distance if it is there's really just I prefer one differential but there is technically two According to some of the textbooks you have ventricular tacac cardia which is going to be very evident here as the wide Qs complexes and again a very similar morphology so we call this monomorphic ventricular tacco cardio when I see wide regular Tac cardia for me it's ventricular
Tac cardia until proven otherwise now while that's being said there is the possibility of psvt so what do I mean by this so if I come back for a second here psvt is proxis Mal super ventricular Tac cardio with abery what the heck does that mean that means that they have psvt which is a narrow regular OC cardio but then you throw in a bundle branch block and the bundle branch block is what makes it look wide and regular but it's it's important to be able to understand that it's not easy to differentiate these two
you can use like different types of criteria like the rato criteria but it's relatively difficult and often times if you treat ventricular attack cardia and it was P psvt you'll be safe but if you treat psvt with abery and it's really ventricular attack of cardia it could actually be dangerous so it's important to remember that it's always vtac until proven otherwise now take the other scenario where they RR interval is abnormal it's not the same distance then I'm thinking about something like ventricular fibrillation when I see this this is ventricular fibrillation it's wide it's irregular
it's erratic this is super scary when you see this one all right another one will be torsades to point so torsa point is usually going to be seen with a patient who has a preceding prolong QT interval so the QT interval will be pretty long and then all of a sudden sh sh sh sh sh you see kind of a polymorphic presentation of ventric Tac cardia so prolong QT followed by a polymorphic presentation of intrical Tac cardia is super suggestive of torsades so for example if I kind of zoom in on one of these areas
here you'll see that it has this constant like ribbon type ofe presence to it and that's super classic of torsades to points all right the last one here is atrial fibrillation with abery again this is basically atra fibrillation we know is a narrow irregular but if you throw in a bundle branch block it makes it wide and regular again I think it's important to remember for vtac viib tors Asda points think about the underlying ca for vtac viib it's probably reent circuits for mardal infarction or heart failure plus increased sympathetic tone as well as potentially
electrolyte abnormalities as well as deox and toxicity in those situations and then for torsades it's usually just hypokalemia hypomagnesemia in combination with prolonged QT interval medications all right that's our our kind of diagnostic Al algorithm now we go into how do we treat Brady arhythmia so we have a patient who comes in their heart rate's less than 60 again I prefer less than 50 and I got to ask myself the question what are the different types now yes there is sinus braic cardia but there's also the blocks that I really want to notice is it
a first degree is it a second degree moitz one is it a second degree moitz 2 is it a third degree a block I want to be able to identify this but the most important thing is if their heart rate's less than 50 and they have features of instability that is an unstable patient that's unstable symptomatic bra cardia what are features of instability come on think about it you're not profusing the brain alter mental status you're not perusing The myocardium angena you're having back flow into the lungs hypoxemia dnia you're having a low blood pressure
or you're having a low blood pressure that's why requiring vasil pressors you're in hypotension you have hypotension or shock in any of those scenarios the patient needs to be given an atropy you give them atropy because it basically blocks the muscar inic two receptors and it helps to to be able to allow for the patient to have a buildup in their heart rate problem is sometimes this will fail and it commonly fails in infranodal AV blocks when the Qs complex is wide so if it fails okay next thing to do is give them epinephrine if
it works great you stop there you don't move any further down this algorithm here and then you go look for the underlying cause so you have to ask yourself is it a beta blocker overdose calcium channel block overdose dexin overdose hyperemia is it ICP crisis is it potentially uh hypothyroidism like mix ademac coma is it some type of myocardial infarction like a right coronary artery occlusion is it lime carditis and you do a full work up and treat the underlying cause but if atropine doesn't work and you're the St patient's still unstable you don't go
work up the underline cause you stabilize them so what's the next thing epinephrine now epinephrine is pretty good and sometimes it will really work if it does work I like to start an epinephrine infusion but even if it doesn't work i' still would consider starting an EP Ander infusion and if you don't want to use that one you can consider other types of infusions such as isoproterenol and dopamine so epinephrine will hit the beta 1 receptors pretty hard it also has again some Alpha receptor isoproterenol is a pure beta 1 receptor so this is actually
my favorite one this can get the heart rate out of stone and dopamine is a pretty good one as well it has a beta 1 receptor activity but it also has some dopamine receptors but these any of these will do now how do I use these I start off with atropine they still have um braic cardia and instability start up an give them an epinephrine push they're still Broc cardic and they're showing signs of instability start them on an infusion you can do epinephrine you can doinol you can do dopamine you're trying to maintain at
least somewhat of a stable heart rate all right you don't want them to decompensate and code while you're doing that you're getting the pads on the patient to past them so you start the infusion gives you time for your team to get the pads onto the patient and start doing transcutaneous pacing so you put the pads on the patient and it's going to send electrical activity and become the Pacer of the heart while you're doing this you're going to give them pain medicine you're going to give them uh sedation and you're going to put a
catheter into their neck or into their clavical area and thread down this Pacer wire into their heart where it will then act as a temporary pacemaker it's called a transvenous Pacer and that's only going to be done in the interum until you can get the patients stable and once they're stable you'll put in a permanent pacemaker for the remainder of their life to prevent any bra cardia in the future all right what about the treatment of Tachi arhythmia so in this type of patient we will talk about the unstable form in a second but for
tthm I want you to think about all the different types at least the ones that we really should address so for psvt proxis super ventricular Tac cardia if they're going really fast which they can they can get heart rates up to 170s 180s 200s it's important to remember for these the first thing that you should do is try to suppress the actual AV node by doing a vagal maneuver because it releases acetylcholine and tries to block those that conduction by hitting the muscarinic 2 receptors and hyperpolarizing them so you do this by maybe having them
bear down valava and see if that works if it doesn't and they don't go back into their native Rhythm then you give them adenosine adenine 6 milligram usually will work and if that doesn't you can try 12 milligrams and it basically will help to shut down the know and reset the heart usually that will work in the situation where the patient it works and then they flip back into psvt multiple times then I would say that you should start this patient on a long-term beta blocker or calcium channel blocker so for beta blocker this would
be things like mopol carvol for calcium channel blocker to be things like delzam of rapel and hopefully it'll prevent the recurrent episodes of psvt and if it doesn't then that's when you consult the patient for electrophysiology study and consider them getting a was called a radio frequency oblation where they burn the bundle of Kent or they burn the abnormal uh Pathways in the AV node for these patients what about atrial flutter and atrial fibrillation all right with atrial flutter and atrial fibrillation again it's important to remember for this one that you're always trying to treat
the underlying cause for this one it's an abnormal pathway the best thing that'll get rid of it is a radio frequency oblation for these it could be a bunch of things it could be a ranr circuit that could be amendable to radio frequency oblation right definitely possible but it's often times other things hypokalemia hypomagnesemia High sympathetic tone right a lot of those Concepts and so you have to treat the underlying cause but in the interum stabilize them so one of the first things that we should do is we should rate control them this is often
times Superior in these patients so this could be beta blockers maybe start them off with some metal LA or some Carval LA and if that's not working you can add on a calcium channel blocker like delam Verapamil and then I have seen in some scenarios where if despite they're on all of these you can add on dioxy if despite all of this the patient is still in atrial fibrillation um so they're not kind of like slowing down or you want to get them out of atrial fibrillation into normal sinus or their native Rhythm that's when
you can go to Rhythm control um often times this would be things like am odone if they have heart failure or sodal if they have something like coronary artery disease I think the big thing to remember is if the patient is developing refractory atrial fibrillation or atrial flutter despite Avid and you know consistent rate and rhym control that's when I would you know refer the patient to an electrophysiologist and consider like a radio frequency ablation where they burn the uh re-entrance circuits around the pulmonary veins or they re they burn the circuit around the caval
trospa dismus and that may be an effective therapy we then go into treatment of ventricular tardia now you may be asking yourself the question Zach you didn't talk about uh sinus tardia again you treat the underlying cause you don't give them any medications you treat the underlying cause you what about multifocal at tardia you treat the underlying cause you treat their COPD right you get rid of the the offlin for the ones that we talked about those actually have specific medical therapies so now let's go to the ventricular Rhythm such as ventricular tacac cardia and
a patient who has stable no features of instability with ventricular tacac cardia often times the best medications here when you see them is to initiate Rhythm control so I like to get them out of this immediately Ami odorant is good for heart failure and I like a lidocaine if I suspect an MI then if I want to prevent them from going back into ventricular attack cardi so let's say I get them on amod they convert to their normal Rhythm I want to prevent them from going back into ventricular hoc cardia and that's where I prefer
like a beta blocker if a patient keeps flipping into vtac or they go into vtac and they lose their pulse and they develop you know they go into cardiac arrest if I get them back I want to refer the patient potentially to an electrophysiologist to consider hey should we potentially do like an aicd um to prevent them if they go into this Rhythm from going into cardiac arrest and so they would implant this in to shock them whenever they go into vac same concept is torsades torsades the underlying cause here is usually hypokalemia hypomagnesemia and
prolong PR QT prolonging medications so discontinue those give them potassium but most importantly give them magnesium four grams of IV magnesium the moment you see this and then again with torsa points usually the big thing is treating the underlying cause but there is certain diseases where tors odda points can actually be more frequent especially if a patient has underlying channelopathies like Long Long QT syndrome and those scenarios if they have recurrent torsades or you they have a you know they go into sudden they develop a cardiac arrest I would potentially refer that patient for um
electrophysiology to consider getting an aicd especially at that Long QT syndrome now we went through all the different types of like staish tacac cardia what if I have a patient who has a unstable Tac cardia so they have a heart R to 100 they have features of inability which is what alter mental status from poor brain profusion Anga for poor poor myocardial profusion poor pulmonary back flow increased pulmonary back flow leading to pulmonary edema in form of disia hypoxia hypotension and maybe even features of shock if they have that what do I do well in
these patients I don't even waste time with medications I get the pads on them I'm going to initiate electrical therapy so the type of electrical therapy you do depends upon the type of arhythmia they have or tack arhythmia if it's Atri flutter Atri fibrillation uh proxis super ventricular attack of cardia or vac these are ones that you can actually cause the AED to sink up with their R waves and you can cardiovert them through that particular process all right so any of these you see these inate unstable you can actually cardio these patients however if
I see torsades this is not something that the AED will do a good job of tracking the rwa for so I won't even try to syn with their actual Rhythm I will just defibrillate them at any point in that actual rhythm all right so that's how we would treat these different types of tacky arrhythmias and again remember this is what we would do to stabilize it but you also have to remember you have to treat the underlying cause last but not least is the treatment of cardiac arrest if a patient comes in right and they
have PA or asyu so what does that mean that means that in both of these they have no pulse because they have no cardiac output right in this particular situ ation PA is they have an organized Rhythm maybe normal sinus or they're Flatline but they have no pulse when you come to a patient no pulse oh they're in paa or asly what is the first thing that you tell them to do the most important thing is to initiate CPR compressions is going to be literally the most important thing because you are now acting as the
heart you are profusing the organs you are perfusing their brain and in this particular scenario how well the compressions are performed will determine the potential long-term complications that these patients may experience so pushing down will squeeze blood out of the heart and then a good time of relaxation will allow for them to fill and compress back down again this is the thing that's maintaining organ profusion while you're doing this other team members should be obtaining good access for medications like epinephrine and potential things like amodine and Etc the other thing is I should have other
team members putting the pads on the patient to assess the Rhythm to see if they need to be shocked usually PA or asy that is not a shock Alor rithm but if they went into vtac or V FIB that is a shock abor Rhythm so you need to have the pads to analyze that after I do CPR for about 2 minutes I'll have everybody come off of the patient we'll take a second we'll look for a pulse assess for a pulse and look at the Rhythm if a pulse is present then you have achieved return
of spontaneous circulation the patient can now terminate from the code no more compressions assess to see if they can follow commands in other words can you give me a thumbs up can you look at me can you communicate unicate with me if they can good they don't really need to undergo targeted temperature management or therapeutic hypothermia if they can't or they have any myoclonic seizure activity they need to be cooled [Music] immediately if during that Rhythm and pulse check they do not have a pulse at that point again assess is it an organized Rhythm do
they have PA are they asy okay if they are you do not Shock that patient you do not defi it's not a shockable rhythm you just give them one milligram of epinephrine and you get back on the chest and start doing compressions and at the same time you and your team members should be thinking about the hes and the t's do they have hypoxia give them oxygen do they have hypotension give them fluid give them vasal pressors do they have acidosis give them bicarb do they have hypoc chemia give them potassium do they have hyperemia
give them calcium give them insulin give them bicarb give them potentially um some type of medication such as albuterol to shift the potassium do they have hypothermia warm them give them warm fluids is it tonon do a paric cardiio synthesis is it attention to authora throw in a chest tube is it a mi give them TPA potentially right is it a PE give them TPA is it toxins give them the antidote if you know or if it's possible to do that and that may prevent them from going back into cardiac arrest or get them out
of cardiac arrest and that's important to remember if you have another patient who you come to and in that code you have no pulse you look at the actual Monitor and you see a wide complex a wide regular it could be vtac right without a pulse or if you see the wide irregular Rhythm and you see viib this is something that you have to be able to differentiate and say hey team members start CPR do good quality compressions get IV and IO access get the pads on the patient let's get the monitor ready to assess
to see if they can analyze it if it's a shockable rhythm after 2 minutes you reassess them if they have a pulse Ros is achieved good if they're they're following no myoc clonus no targeted temperature management if they are not following if they have myoc clonus targeted temperature management if they do not have a pulse and they are in vtac or they are in V FIB that is a shockable rhythm you defibrillate them give them a milligram of epinephrine get back on the chest and start start pcpr the next time you do a rhythm and
pulse check if they're still in vtac or viib you shock them and an alternative to give that you can flip back and forth with besides epinephrine is am odorum because that may help to reset the electrical activity either way after every single time you give them a med and defibrillate them you get back on the chest and you continue the CPR thinking about what is the causes of this patient going into this deadly type of Rhythm my friends this is arhythmia it was a monster I really hope that it made sense I really hope that
you guys enjoyed it I love you I thank you and as always until next time [Music]
Related Videos

37:58
Atrial Fibrillation | Clinical Medicine
Ninja Nerd
68,029 views
36:08
ECG Interpretation | Clinical Medicine
Ninja Nerd
302,071 views

1:43
20241211 (audio)
The Eighth Wonder
7,567 views

18:31
Understanding Arrhythmias
Zero To Finals
102,551 views
19:55
Supraventricular arrhythmias: Pathology re...
Osmosis from Elsevier
34,590 views
44:57
Diabetes Mellitus | Clinical Medicine
Ninja Nerd
266,803 views

16:45
The Tipping Point I Got Wrong | Malcolm Gl...
TED
646,454 views

12:49
Old Soldier Meets Young Soldier | The Gap ...
LADbible Stories
39,603,465 views

27:11
You're Probably Wrong About Rainbows
Veritasium
4,474,301 views

58:20
Congestive Heart Failure | Clinical Medicine
Ninja Nerd
286,351 views

1:16:07
Lecture 1: Introduction to Superposition
MIT OpenCourseWare
7,663,698 views

5:37
What staying up all night does to your bra...
TED-Ed
1,858,209 views
12:14
Most Common ECG Patterns You Should Know
Rhesus Medicine
1,627,135 views

2:40:46
Antiarrhythmic Drugs
Ninja Nerd
331,229 views
28:39
Hyperlipidemia | Clinical Medicine
Ninja Nerd
59,290 views

17:46
Heart Conduction System & ECG (EKG)
Siebert Science
113,855 views

4:07
Gabor Maté Goes Off On Jordan Peterson
The Mind Fortress
159,988 views

20:05
How To Lower Your Blood Pressure (Cardiolo...
Talking With Docs
1,598,029 views

52:22
Coronary Artery Disease | Clinical Medicine
Ninja Nerd
186,998 views

40:50
Cardiac dysrhythmias (arrhythmias) (common)
Dr Matt & Dr Mike
149,612 views